Uncategorized

August 8, 2017. Ragweed Pollen Readiness: 3 Keys to Prepare for Fall Allergies
Ragweed Pollen and Fall Allergies:
Ragweed pollen is considered the biggest trigger of fall allergies. Ragweed pollen will flood the air in metropolitan Philadelphia and Southern New Jersey over the next few weeks, according to Dr. Donald Dvorin, the region’s only official pollen, ragweed, and mold spore counter. Dr. Dvorin is watching the ragweed plants in the Delaware Valley mature. Based on more than two decades of historical data as well as ideal growing conditions (this summer’s hot and rainy weather conditions) a robust ragweed pollen season is expected.
August marks the beginning of the end of summer. For many it is a time for relaxing, “last chances” for summer fun with family, and vacations. August also brings ragweed pollen and the onset of fall allergies. The Asthma Center Board-Certified Allergists recommend taking 3 Key Steps now to prevent suffering (and sneezing) through fall allergy season!
3 Key Steps to Prevent Fall Allergies
- Implement your personal Allergy Action Plan now.
Be sure to begin your allergy and asthma medications before your symptoms start (including the use of intranasal corticosteroid sprays). This is one of the most important measures you can take to minimize seasonal allergy symptoms.
Advisory for current patients of The Asthma Center: We recommend reviewing and updating your Allergy Action Plan with your board-certified allergist every three months.
2. Know your level of pollen sensitivity and monitor pollen levels.
To find out if you are allergic to ragweed, Allergy Skin Testing is one of the most reliable methods to determine allergy sensitivity, particularly when correlated with your personal history. Free subscribers of The Asthma Center’s daily email receive pollen, mold, and ragweed counts direct to their inbox.
Advisory for current patients of The Asthma Center: Sensitivity to pollen and molds (including ragweed) can change over time. We recommend reviewing your allergic sensitivity with your board-certified allergist every three months and testing for allergies every two years.
3. Keep pollen and mold spores out of your nose, eyes, ears, lungs and home.
- Wear long sleeves and long pants when mowing the grass or raking leaves. Be sure to shower & wash your hair afterwards.
- Limit time outdoors during the early morning hours when the most pollen is released. Be mindful that molds release mold spores throughout the day. Learn more
- Sleep with windows closed and drive with windows up.
- Wear wrap-around sunglasses or glasses outdoors to limit exposure of pollen to your eyes.
- Avoid wearing contact lenses, or switch to daily disposable contacts to avoid allergens building up on the lenses.
- Beware of tracking pollen and mold spores into your home from overlooked sources that may “sneak” in on kids’ shoes and clothing, pets especially after playing outside in the grass and leaves, and on morning newspaper sleeves.
- Shower and wash your hair after extended outdoor exposure. Wash your hands and face frequently, including eyebrows.
- Change your pillowcase often.
A Board-Certified Allergist Can Help with Ragweed and Fall Allergies & Allergic Asthma
At The Asthma Center, our allergists and pediatric allergists help our patients manage their ragweed pollen and fall allergies and allergic asthma by determining what weed pollen and molds cause symptoms. For example, we identify whether ragweed pollen and or which local molds (including Cladosporium, Ascosopres, Alternaria, Basidiospores, and Epicoccum) trigger allergy and asthma symptoms by using minimally invasive in-house diagnostics, like allergy skin testing, needle free allergy skin testing and breathing tests. Pairing these results with local knowledge of allergy triggers like pollen, ragweed and mold, our allergists develop personalized plans that treat not only the symptoms but also the cause of allergies. And because allergy and asthma symptoms often spike with pollen, ragweed, and mold spore counts, we know exactly when to adjust medications – providing more relief when conditions are bad and less medication every time else.
The allergists, pediatric allergists, and asthma specialists at The Asthma Center treat patients in 9 convenient locations throughout the Delaware Valley including Philadelphia (Center City Philadelphia, Society Hill Philadelphia, Northeast Philadelphia), The Main Line – Montgomery County (Bala Cynwyd – Lower Merion), Bucks County (Langhorne), and South Jersey (Mt. Laurel, Woodbury, Princeton – Hamilton, Forked River).
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
For interviews and tours of the Delaware Valley’s only National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com
More Info

July 28, 2017. Thunderstorm Asthma – Allergies: More Pollen, More Mold, More Symptoms
Thunderstorm Asthma – Allergies
Over the past thirty years, numerous researchers have confirmed that “thunderstorm asthma – allergies” (increases in asthma and allergy symptoms following thunderstorms) are real.
The “dog days of summer,” those hot and humid days in late July and August present the perfect conditions for unsettled weather which can “break” the humidity with rain and cooler temperatures. Many individuals who have asthma and allergies expect these weather changes to also usher in a break from symptoms. The Asthma Center’s board certified allergists and pediatric allergists also confirm that thunderstorms can have the opposite effect by triggering more allergic asthma and respiratory allergy symptoms.
What Is Thunderstorm Asthma – Allergies?
Most people think of a “thunderstorm” as any storm with rain, thunder and lightning. Thunderstorms are very common, and according to the National Oceanic and Atmospheric Administration (NOAA), at any given moment, somewhere around the world, approximately 2,000 thunderstorms are in progress. While thunderstorms may seem simple, each event is a complicated interaction of air, water, and electricity.
Thunderstorm Asthma – Allergies occurs when thunderstorm activity triggers flares in asthma (coughing, wheezing, shortness of breath or chest congestion) and/or allergies.
The connection between thunderstorms and increased asthma and allergy symptoms was first recognized in the 1980s. Over the ensuing years, a number of researchers have confirmed this phenomenon including increased emergency room visits for asthma following thunderstorms. In fact, deaths due to increased asthma after thunderstorm activity occurred in Melbourne, Australia (9 deaths in November 2016) and in Kuwait (5 deaths in December 2016.)
Most recently, findings published in the American Meteorological Society’s Journal of Applied Meteorology and Climatology explored the complicated relationship of thunderstorm activity with increased pollen, thunderstorm asthma and respiratory allergy.
Thunderstorms Bring More Pollen, More Mold Spores & More Symptoms
For more than two decades, The Asthma Center’s official pollen, ragweed and mold spore counter, Dr. Donald Dvorin has observed first hand the increase of pollen, ragweed, and mold spore counts following thunderstorm activity in metropolitan Philadelphia and Southern New Jersey. As Dr. Dvorin has stated on many occasions, weather conditions play an important and complex role in the volume of pollen, ragweed, and mold spores that fill the air each day. Rain and falling temperatures can clear the air and can even disturb the pollen process. Thunderstorms on the other hand, which are accompanied by lightning, winds and heavy rains–affect the process differently. First, winds lift, carry, and toss pollen about, sometimes violently. Lightning indicates a change in the movement of atmospheric electrical charges which may cause further anomalies in pollen release; when combined with winds, this can result in more pollen in the air with all of it traveling further.
The most recent published findings suggest that pollen molecules may actually absorb water in the atmosphere before “exploding” and releasing pollen particles with great force and density.
Molds thrive with increased moisture. It is no surprise, then, that there is a connection between increased mold allergy symptoms and storms, which include thunderstorms, rain, tropical storms, and hurricanes.
In fact, in April, 2017, a study in the Journal of Environmental and Public Health reported findings from two researchers on the connections between Hurricane Irene in 2011 and Hurricane Sandy in 2012 and positive reactions to allergy skin testing to molds. The researchers reviewed the medical records of several hundred individuals living in New Jersey, and found that post-hurricane allergy skin tests revealed an increased allergic reaction to molds.
Three Ways To Reduce Thunderstorm Asthma – Allergies
- Minimize Time Outdoors Before and After Thunderstorms
While thunderstorms can “pop up” at any time without warning, cloud formations, darkening sky, lightning, and abrupt changes in wind gusts are all clues that a thunderstorm may be forming. The rhyme “Red sky at night, sailors’ delight; Red sky in morning, sailors’ warning” is another clue. As seen in this photo (courtesy The Asthma Center’s friend, Bill Fluehr) which captures the morning sun along the Delaware River, a “red sky at morning” is caused when the sun hits clouds in our region.

2. Monitor Pollen, Ragweed, and Mold Spore Counts
Knowing the pollen, ragweed, and mold spore counts before and after thunderstorms can be invaluable in planning daily activities and reducing the impact of exposure to your specific allergy triggers. In the Delaware Valley, The Asthma Center’s official pollen, ragweed, and mold spore counts are available via free subscription email, on our website, and social media.
3. Activate your Asthma & Allergy Action Plan
A personalized Asthma & Allergy Action Plan will include both a routine, day-to-day plan for individuals with asthma and allergies as well as a written plan to follow in the case an asthma attack or flare up in allergy symptoms. The Asthma Center allergists work with each patient to customize each individual’s Asthma & Allergy Action plan so that patients know when to adjust medications – providing more relief when conditions are bad (after thunderstorm activity when pollen, ragweed, and mold spores may dramatically increase) and less medications when environmental triggers are absent.
Special Note for Individuals with Thunderstorm Asthma: Carry Your Rescue Inhaler At All Times
A Board-Certified Allergist Can Help with Thunderstorm Asthma – Allergies
At The Asthma Center, our allergists and pediatric allergists help our patients manage increases in symptoms after thunderstorms by first determining what causes an individuals asthma and allergy symptoms. For example, we identify which local pollen, ragweed, and molds trigger allergy and asthma symptoms by using minimally invasive in-house diagnostics, like allergy skin testing including needle free allergy skin testing and breathing tests. Pairing these results with local knowledge of allergy triggers like pollen, ragweed and mold, our allergists develop personalized plans that treat not only the symptoms but also the cause of allergies. And because allergy and asthma symptoms often spike after thunderstorms, we know exactly when to adjust medications – providing more relief when conditions are bad and less medication every time else.
The allergists, pediatric allergists, and asthma specialists at The Asthma Center treat patients in 9 convenient locations throughout the Delaware Valley including Philadelphia (Center City Philadelphia, Society Hill Philadelphia, Northeast Philadelphia), The Main Line – Montgomery County (Bala Cynwyd – Lower Merion PA), Bucks County (Langhorne PA), and South Jersey (Mt. Laurel NJ, Woodbury NJ, Hamilton NJ, Forked River NJ).
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
For interviews and tours of the Delaware Valley’s only National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com
More Info
July 11, 2017. Travel with Allergies & Asthma: Tips to Avoid Symptom Detours
Travel with Allergies & Asthma: Tips to Avoid Symptom Detours
Summer is a special time for making memories including travel and vacations. It might be a daytrip, a weekend getaway, a family vacation or reunion, a road trip across the United States (or to a particular landmark or region), a longer trip abroad, or a “bucket list” cruise or adventure. While some diversions can add to the fun of traveling, detours caused by flare ups in allergies, asthma, and sinus problems can cause misery for everyone. The Asthma Center’s board certified Allergists have created the following Travel with Allergies & Asthma checklist to help you and your family enjoy healthy and safe outings, travel and vacations!
Before Travel: Allergies & Asthma Checklist
- Visit your specialist. The board certified Allergists & staff of The Asthma Center can help you get ready by reviewing your personal Action Plan & special travel needs. For example, individuals with asthma may be unaware that nebulizers are available in extremely small, lightweight, battery-operated, & tubeless units, which can fit into a purse or small travel bag, such as the Omron MicroAir nebulizer. We can help you find the unit that’s right for you.
- Prepare a list of current medical conditions (including food & medication allergies) & medications.
- Prepare & pack sufficient quantities of prescription & over-the-counter medications including all back up medications. Check expiration dates.
- Research accommodations. AllerPassMD (edited & analyzed by a board certified allergist provides listings and ratings for hotel rooms & staterooms) is one resource providing hotel ratings on Indoor & Outdoor Allergens as well as Contactants (hair & body products.) Request smoke free rooms with air filters & dust mite proof bedding when booking your lodging.
- Research restaurants. Find food allergy aware restaurants using SafeFare (created by Food Allergy Research & Education (FARE))
- Research your vacation location regarding, air quality & environment, language, nearest medical facility, and pharmacy locations.
- Check your insurance policy regarding coverage and, if applicable, purchase and review extra travel medical benefits.
- For those with severe allergy/anaphylaxis, consider purchasing an Allergy Medic Alert Bracelet. When engraving, be as specific as possible in identifying your allergies.


- Review pre flight instructions to prevent or lessen Eustachian Tube Dysfunction (problems related to ear pressure such as pain, fullness, hearing difficulties) – An example of The Asthma Center Allergists’ Pre Flight Instructions for Eustachian Tube Dysfunction might include:
The above instructions are only an example. The use of Afrin, decongestants, and/or prednisone must be discussed with a board certified Allergist. Schedule an Appointment
Dodge Detours: Avoiding Allergies & Asthma With Travel
- Carry your list of conditions, medications, and emergency medications everywhere you go.
- Avoid tobacco smoke exposure and always ask for smoke-free hotel room with air filter and dust mite proof bedding
- Use hand sanitizer and wash your hands frequently
- Know the closest emergency services or hospital locations
No Place Like Home: Allergies & Asthma De-Briefing Guide
- Visit your specialist for follow-up care if you experienced any allergic reactions, asthma flares, and/or anaphylaxis while traveling and if necessary make adjustments to your Action Plan.
- When unpacking, ensure you returned home with all your medications and refill medications as needed.
- Note what was successful and/or unsuccessful on this trip regarding your asthma, allergies and/or sinus problems. If applicable, write online review of restaurants and/or hotel accommodations to share your experiences with others who have allergies and asthma.
Travel with Epinephrine (EpiPen or AuviQ)
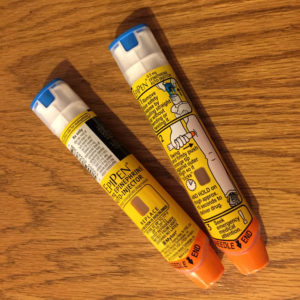
- Visit your specialist if you require special documentation and to review your personal Action Plan
- When flying, request that your epinephrine be visually inspected, not scanned
- Always carry your epinephrine (do not pack in luggage which will be checked because it will be handled by others and may be lost, delayed or damaged )
- Check the effective date of your epinephrine.
- Know the closest emergency services or hospital locations
A Board-Certified Allergist Can Help Travel and Allergies, Asthma and Sinus Problems
At The Asthma Center, our allergists and pediatric allergists help our patients plan for travel to minimize allergies, asthma, and sinus problems. For example, we identify which local pollen and molds trigger allergies, asthma, and sinus symptoms by using minimally invasive in-house diagnostics, like allergy skin testing and breathing tests. Pairing these results with local knowledge of allergy triggers like pollen, ragweed and mold, our allergists develop personalized plans that treat not only the symptoms but also the cause of allergies. And because allergy and asthma symptoms often spike with mold spore counts, we know exactly when to adjust medications – providing more relief when conditions are bad and less medication every time else.
The allergists, pediatric allergists, and asthma specialists at The Asthma Center treat patients in 9 convenient locations throughout the Delaware Valley including Philadelphia (Center City Philadelphia, Society Hill Philadelphia, Northeast Philadelphia), The Main Line – Montgomery County (Bala Cynwyd – Lower Merion PA), Bucks County (Langhorne PA), and South Jersey (Mt. Laurel NJ, Woodbury NJ, Hamilton NJ, Forked River NJ).
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
For interviews and tours of the Delaware Valley’s only National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com
More Info

June 28, 2017. Mold Spores Galore: Extreme Mold Allergies in Delaware Valley
Mold Spores Galore: Extreme Mold Allergies in Delaware Valley
Mold allergy, allergic reactions to mold spores, are on the rise in the United States causing misery for perhaps one in three individuals with allergies and/or allergic asthma. Last week in the Delaware Valley alone, Dr. Dvorin reported extreme outdoor mold counts for several consecutive days, with nearly 9000 mold spores per cubic meters of air / 24 hours. The reported high mold counts may provoke severe allergic and asthma symptoms for people in Philadelphia and South Jersey.
Drawing on decades of expertise in identifying, evaluating and treating the common and uncommon manifestations of mold allergy, The Asthma Center’s board-certified allergists present Mold Spores Galore: Extreme Mold Allergies in Delaware Valley.
Mold Allergy Symptoms
Virtually no environment is without molds which release mold spores. Too small to be seen by the naked eye, mold spores are found in every breath we inhale, and may also enter the body through the eyes, ears, mouth, and skin.
Adults and children with mold allergies may experience the typical symptoms of allergy such as sneezing, nasal congestion, and/or itching of the nose, itchy and watery eyes, itchy ears and/or hives (skin rash.) Exposure to mold spores can also provoke flares of asthma, chronic sinusitis, and headaches, including migraines. Less common, severe allergies to mold spores include allergic bronchopulmonary aspergillosis (ABPA) and allergic fungal sinusitis (AFS.)
Mold Allergy and Outdoor Mold Counts
Molds, also known as fungi, produce spores and other fungal particles. Outdoor mold spores play a major role in causing most mold allergy symptoms. Like pollen, mold spores are airborne and become abundant in the warmer weather months. Unlike pollen, which typically is released in the greatest numbers early in the day, mold spore release depends three factors: 1) type of mold present, 2) heat and 3) humidity. “Dry air” spores (xenophilic) such as Cladosporium or Alternaria release the most spores during the afternoon hours when the weather conditions are hot and dry. “Wet air” spores (hydrophilic), such as Ascospores and Basidiospores release the largest numbers of spores during pre-dawn hours when there is high humidity.
Delaware Valley’s Outdoor Mold Spore Counts

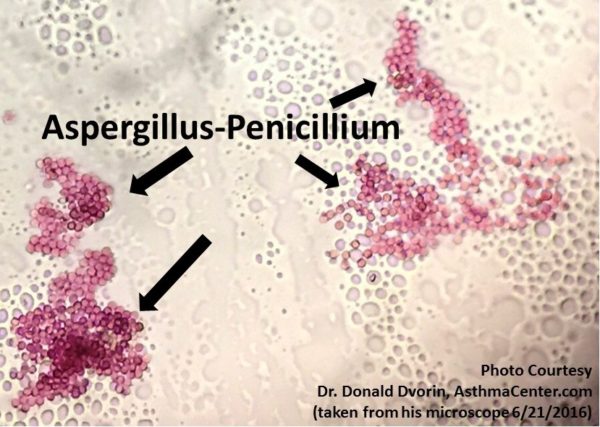
Pollen and mold spore particles have distinct shapes and are easy to distinguish from each other under the microscope. However, mold spores and other fungal particles are very small and can be challenging to differentiate between the species. The Asthma Center’s Dr. Donald Dvorin’s training, experience and certification by the National Allergy Bureau (NAB) combine to bring the Delaware Valley the only official mold spore count for metropolitan Philadelphia and Southern New Jersey.
For those with mold allergies, knowing the daily mold count is essential in order to reduce the impact of exposure to outdoor mold spores, for planning daily activities and following Allergy & Asthma Action Plans (increasing or decreasing medications.) In the Delaware Valley, The Asthma Center’s official pollen, ragweed, and mold spore counts are available via email, on our website, and social media.
In metropolitan Philadelphia and Southern New Jersey, molds appear in the early spring and persist throughout the summer and fall seasons. There is no “peak season” for mold spores. Dr. Dvorin has observed that the highest levels of mold spores, which may provoke extreme symptoms, occur from midsummer through the late fall. During winter months, outdoor mold spores reduce significantly – especially if snow covers the ground.

Dr. Dvorin’s historical mold data reveals that Cladosporium is the predominant mold spore in our region’s air. Other common molds for our region include Ascospores, Alternaria, Basidiospores, and Epicoccum.
Dr. Dvorin also notes that the unusual mold spores of Aspergillus and Penicillium are frequently present in the air of the Delaware Valley. These mold spores can cause severe allergic reactions in the lungs (allergic bronchopulmonary aspergillosis [ABPA] ) and sinuses (allergic fungal sinusitis [AFS.] ). When Aspergillus and Penicillium mold spores are elevated, The Asthma Center issues an Unusual Mold Alert for metropolitan Philadelphia and South Jersey. Subscribe to receive these alerts with daily mold spore counts direct to your inbox!
Other molds species observed in our region by Dr. Dvorin include Botrytis, Cercospora, Curvularia, Drechslera, Fusarium, Nigrospora, Oidium, Periconia, Pithomyces, Polythrincium, Rusts, Smuts, Stemphylium, and Torula.
Top 5 Ways to Reduce Mold Spore Exposure & Mold Allergies
- Avoid uncut fields and piles of damp leaves if possible.
- Make sure water drains away from your home (not toward the basement or foundation). Vent dryers to the outside-not indoors!
- Monitor indoor humidity levels and make your home less mold-friendly by using dehumidifiers and air conditioners. Keep indoor humidity between 35% and 50%. (Inexpensive meters for measuring humidity in a home can be purchased at a hardware store.)
- Identify the source of mold and remove it before it spreads. If you spot mold in your home on a hard surface –such as glass, plastic or tile—clean it with a bleach solution, soap and water, or a commercial product. For mold on drywall, seek professional advice.
- Do not procrastinate! Acting promptly is a critical component of mold prevention. If a spill or leak leaves a rug wet, dry it within 48 hours to keep mold from growing. Be sure to not delay from cleaning gutters, because the damp leaves serve as a breeding ground for mold.
Lawn Allergy: Mold & Cut Grass
Mowing your lawn to reduce grass pollination and limiting your exposure to grass pollen are both important steps in avoiding the misery of allergies. In addition to grass pollen triggering allergy symptoms, many individuals experience typical allergy symptoms such as sneezing, itchy watery eyes, nasal congestion, and even wheezing when exposed to the smell of freshly cut grass. Allergic reactions triggered by the smell of freshly cut grass are likely from the non-pollen parts of the grass, which also contain allergenic proteins or outdoor molds, which have been stirred up by the mowing process. Concentrations of these allergy triggers dramatically escalate for a short period of time during and immediately after mowing. For more tips on reducing exposure to outdoor molds when mowing the lawn, read The Asthma Center’s Allergy-Friendly Lawn & Grass Guide.

Outdoor Mold Prevention Tip: If you are seeing mold growing on your mulch, be sure to check the thickness of the layer of mulch. Mulch layered thicker than 3 cm allows for molds to grow, repelling water from reaching the roots under the mulch.
Storms Kick Up Mold Allergies
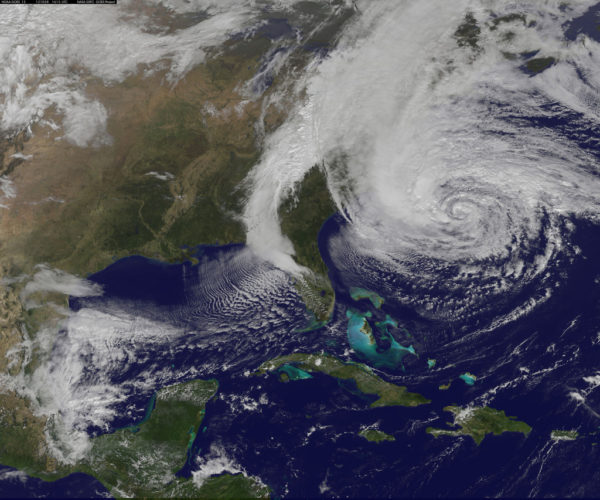
Molds thrive with increased moisture. It is no surprise, then, that there is a connection between increased mold allergy symptoms and storms, which include thunderstorms, rain, tropical storms, and hurricanes.
In fact, in April, 2017, a study in the Journal of Environmental and Public Health reported findings from two researchers on the connections between Hurricane Irene in 2011 and Hurricane Sandy in 2012 and positive reactions to allergy skin testing to molds. The researchers reviewed the medical records of several hundred individuals living in New Jersey, and found that post-hurricane allergy skin tests revealed an increased allergic reaction to molds.
Mold Triggers Allergic Asthma
Mold allergy is recognized as an important trigger for Allergic Asthma. A board-certified Allergist plays a crucial role in identifying which molds provoke asthma symptoms in order to develop a personalized Asthma Action Plan. A comprehensive evaluation for mold allergy and allergic asthma includes, but is not limited to, allergy skin testing, review of environmental exposures, specialized pulmonary function testing, and a physical examination.
What is ABPA (Allergic bronchopulmonary aspergillosis)?
Allergic bronchopulmonary aspergillosis (ABPA) is an allergic reaction in the lung to Aspergillus fumigatus. Reactions to this fungus are rare in individuals with normal immune systems. Individuals with asthma or cystic fibrosis are among those commonly affected by ABPA. If you have asthma, one of the first noticeable symptoms may be a progressive worsening of your asthma symptoms including coughing, wheezing, and shortness of breath. Other allergic conditions which may be present include nasal allergies (allergic rhinitis), sinusitis, and skin allergies (atopic dermatitis/eczema and urticaria/hives). Treatment usually includes oral corticosteroids and sometimes oral anti-fungal treatments. Individuals with ABPA are usually followed closely by their physician.
What is AFS (Allergic fungal sinusitis)?
Allergic fungal sinusitis (AFS) is the most common fungal infection associated with chronic sinusitis. This condition often occurs in people with nasal polyps and sinus disease. It is usually resistant to conventional medical and surgical treatments. Tissue within the sinuses is often covered with characteristic thick gel-like discolored mucus filled with allergy cells (eosinophils). This gel is often described as “allergic mucin” and often contains fungal elements when properly stained and examined microscopically. Treatment of allergic fungal sinusitis includes surgery, oral and nasal corticosteroids, allergy injection therapy, leukotriene modifiers, antihistamines and oral decongestants. Unfortunately, oral antifungal treatment is usually not effective.
Indoor Mold Allergens
Mold allergens associated with mold spores and other fungal elements can be a major source of indoor allergens, particularly in home where damp or wet areas exist. Areas of mold growth are often difficult to detect, hiding under floors or behind walls.
The mixture of mold spores seen indoors includes Penicillium, Aspergillus, and Cladosporium. Unique molds like Stachybotrys may be found in some indoor settings where extensive water damage has occurred. If molds are suspected, special culture techniques and air sampling specimens may be done. A thorough inspection may be required by experts in environmental contamination and mold remediation.
There have been many claims made regarding connections between damp environments and health effects. Possible reasons for these connections include: allergic reactions, direct irritation by fungal mold elements, toxins released from molds (Aspergillus, Fusarium, Penicillium, Stachybotrys): volatile organic compounds (VOCs), or other immune responses stimulated by mold. Individuals with exposure to damp environments often present with symptoms of congestion, coughing, mucous discharge, headache, shortness of breath, eye itching, dizziness, restless legs, fatigue and abdominal pain. Most individuals with exposure to mold contaminates do not have typical allergic symptoms. Whether all indoor molds produce health problems beyond allergic reactions is still widely debated. Therefore, the presence of mold or mold derived toxins in an indoor environment does not necessarily mean there are associated effects on health.
A Board-Certified Allergist Can Help with Mold Allergy & Allergic Asthma
At The Asthma Center, our allergists and pediatric allergists help our patients manage their mold allergies and allergic asthma by determining what molds cause symptoms. For example, we identify which local molds (including Cladosporium, Ascosopres, Alternaria, Basidiospores, and Epicoccum) trigger allergy and asthma symptoms by using minimally invasive in-house diagnostics, like allergy skin testing and breathing tests. Pairing these results with local knowledge of allergy triggers like pollen, ragweed and mold, our allergists develop personalized plans that treat not only the symptoms but also the cause of allergies. And because allergy and asthma symptoms often spike with mold spore counts, we know exactly when to adjust medications – providing more relief when conditions are bad and less medication every time else.
The allergists, pediatric allergists, and asthma specialists at The Asthma Center treat patients in 9 convenient locations throughout the Delaware Valley including Philadelphia (Center City Philadelphia, Society Hill Philadelphia, Northeast Philadelphia), The Main Line – Montgomery County (Bala Cynwyd – Lower Merion PA), Bucks County (Langhorne PA), and South Jersey (Mt. Laurel NJ, Woodbury NJ, Hamilton NJ, Forked River NJ).
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
For interviews and tours of the Delaware Valley’s only National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com
More Info

June 21, 2017. Summer Camp for Kids with Allergies and Asthma: Blueprint for Fun
Summer Camp for Kids with Allergies and Asthma: Blueprint for Fun
It’s time for Summer Camp! The Asthma Center’s board-certified allergists have prepared the following guide, Summer Camp for Kids with Allergies and Asthma, to help parents and kids in the Delaware Valley get camp-ready for summer fun and making memories with friends.
Allergy & Asthma Action Plan
Preparation is the foundation of any summer camp experience, but this is especially true for children with allergies and asthma. No two children are alike, so pre-camp planning needs to be tailored to each child’s unique history and diagnoses. Our board-certified pediatric allergists meet with parents and children every year to help them create an appropriate Allergy & Asthma Action Plan in order to ensure a happy and safe summer camp experience for kids who may have:
- allergies to pollen, molds, and/or dust
- asthma
- food allergies and/or oral allergy syndrome
- bee sting allergies
- other insect sting allergies and reactions to insect bites
- poison Ivy, Oak, & Sumac reactions
The first step in creating an Asthma & Allergy Action Plan is identifying and listing your child’s triggers, symptoms and conditions. A written plan should cover not only current medication and allergies but also what instructions to follow in the event of an escalation of symptoms or an emergency.
Walking through an allergist-approved Action Plan with summer camp medical staff and camp leaders ensures that the camp staff understand how best to react in an emergency situation, and allows you as the parent to have confidence in the medical care available to your child while they are away from home. For example, if your child carries an epinephrine auto-injector (Epi-Pen, Jr; Auvi-Q), review your child’s Anaphylaxis Action Plan carefully with camp staff, and ask if which staff members are trained to administer epinephrine (and/or other emergency medical care.) Finally, it also can be useful to inquire how the camp has handled allergies, asthma, and reactions to foods or bee stings in the past.
Pre-Camp Medication Tip for Parents:
Summer is not the time to take a break from allergy and asthma medications. Visit your allergist well in advance to review medications. Before a child leaves for camp, make sure sufficient quantities of medications are available and check expiration dates.
Summer Camp for Kids with Allergies to Pollen, Molds, and/or Dust

For kids with allergies to pollen, molds, and/or dust, avoiding exposure to triggers that may cause allergy symptoms to flare can be challenging with outdoor activities while at summer camp. A board-certified pediatric allergist can identify a child’s specific allergy triggers through allergy skin testing, and provide a written Allergy Action Plan for both kids and camp staff. Ask what measures, if any, are followed to reduce allergen exposure. For example, are mold-inhibitors used to keep sleeping areas such as tents and cabins free of mold growth? What measures are used to keep dust exposure at a minimum?
Summer Camp Pollen and Mold Count Tip for Parents:
Ask if medical staff follow pollen, ragweed and mold spore counts for it’s geographic area. Knowing the daily pollen, ragweed, and mold spore counts can be invaluable in planning daily activities and following a child’s Allergy Action Plan (increasing or decreasing medications) and reducing the impact of exposure to a child’s allergy triggers. In the Delaware Valley, The Asthma Center’s official pollen, ragweed, and mold spore counts are available via email, on our website, and social media.
Summer Camp for Kids with Asthma
An Asthma Action Plan will include both a routine, day-to-day plan for kids with asthma and a written plan to follow in the case of an asthma flare. The Asthma Center specialists meet each summer with both parents and kids to discuss asthma action plans including the best ways to prevent asthma attacks while away from home and addressing any questions from children (or parents.) Talking with children who have asthma and answering any questions ahead of time may help “settle their nerves” so they can enjoy their summer experience.
Parents who are concerned about the capability of a specific camp in meeting their child’s asthma needs can also consult with their specialists regarding options, alternatives and “Asthma Camps.” (See list of local Asthma Camps at the end of this blog.)
Summer Camp Asthma Tip for Parents:
Be sure that camp staff know how to contact your child’s asthma specialist in the event of an emergency or asthma flare.
At The Asthma Center, one of our specialists is always on call – if your child needs help, a doctor who knows their medical history will be able to assist remotely.
Summer Camp for Kids with Food Allergies & Oral Allergy Syndrome

Food allergy symptoms can occur within several seconds or hours following food injection, although most reactions occur within the first 2 hours. The following symptoms can occur singly or in combination: Hives; swelling; eczema; itching of the mouth, throat, skin, palms, soles, or genitals; feeling of warmth; feeling of doom; vomiting; diarrhea; abdominal pain; cramping; nasal congestion; shortness of breath; chest tightness; cough; congestion (It is uncommon to see respiratory symptoms alone without gastrointestinal or skin symptoms.), dizziness, feeling faint, and passing out. Aside from the physical reactions, food allergies clearly affect the quality of life of affected individuals and their psychological welfare, especially of children. The “Big 8” (most common) triggers of food allergy are:
- milk
- eggs
- fish
- crustacean shellfish
- tree nuts
- peanuts
- wheat
- soybean.
Oral Allergy Syndrome is a type of food allergy which occurs in children (and adults) who have seasonal hayfever (allergy) symptoms and experience allergic symptoms in and around the mouth after eating certain foods including vegetables, nuts, seeds, and/or fresh fruits.
A board-certified allergist can help identify the specific triggers of both food allergies and/or oral allergy syndrome. Once a triggering food is identified, the best prevention is avoidance. However, for kids with food allergies, a Food Allergy Action Plan is essential for summer camp. A Food Allergy Action Plan, signed by a physician, should:
- outline step-by-step treatment recommendations for allergic reactions and/or anaphylaxis in the case of accidental exposure; and
- include emergency contact information.
To minimize stress while kids with food allergies are away from home at summer camp, provide multiple copies of your child’s Food Allergy Action Plan to the camp, and to your child, and discuss the plan with both camp staff and your child.
Summer Camp Food Allergy Tip for Parents:
If your child’s allergy requires an epinephrine auto-injector (EpiPen, Jr; Auvi-Q), and they are old enough to carry it with them, make sure they understand how to use it – and in what situation.
Stinging Stuff: Allergies to Bee Stings, Insects & Insect Bites

Insects such as bees, wasps, yellow jackets, hornets, and fire ants inject venom into the skin by “stinging” while other insects such as mosquitoes, fleas, black flies and ticks, use their saliva or bodies to produce reactions by “biting” and contact with skin. While most reactions to stinging and biting are mild to moderate, some adults and children experience sudden, severe and life-threatening reactions from stinging insects. Children who have been diagnosed with severe reactions to stinging insects should have an Anaphylaxis Action Plan, carry an epinephrine auto-injector, and wear an ID bracelet, anklet or necklace which identifies he/she as allergic to stinging insects.
Top 5 Ways to Reduce Risk of Insect Stings and Bites
- Wear shoes outside at all times.
- Wear white, green, tan, or khaki colors. Bright colored clothing is more likely to attract insects.
- Wear fitted clothing. Insects may become trapped in over-sized or loose, flowing clothes.
- Stay still when an insect is approaching. Never slap at an insect. Insects will not sting unless frightened or antagonized, so stay as calm and relaxed as possible.
- Avoid wearing scents, such as perfumes, hair sprays, and suntan lotion, which often attract insects. Keep foods and/or drinks covered while outside as these aromas may also attract insects.
If Attacked by Stinging Insects:
- Cover face with arms, and if possible, run and find shelter. Kids should find an adult or counselor immediately.
- Do not grab or squeeze any stinger attached to skin because this may cause more venom to inject into the wound.
- Remove a stinger and/or “venom sac” carefully by scraping the spot with your fingernail.
- Wash the area of the sting thoroughly with soap and water, and apply an antiseptic.
- Use cold compresses to the the site of sting for 15-20 minutes followed by Calamine lotion to reduce swelling and irritation.
- An oral antihistamine may be required to reduce itching.
Seek medical attention immediately if you notice signs of an allergic reaction such as widespread swelling, chest tightness, or dizziness.
Bee Sting Allergy Tip:
The Asthma Center’s board certified allergists recommend that any individuals who are sensitive to insect venom should be treated with venom injections, which has been proven to be effective in greater than 95% of individuals.
Lone Star Tick Advisory:
Did you know that red meat allergy can be triggered by bites from the Lone Star Tick, a variety of tick that is active and prevalent in our region? Learn all the facts in our recent blog Allergic to Red Meat? Lone Star Ticks to Blame.
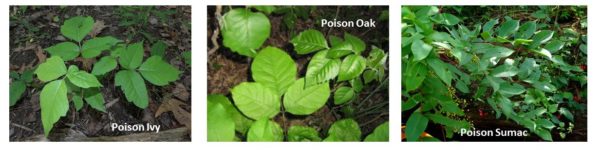
Avoid the Itch: Poison Ivy, Poison Oak, and Poison Sumac Reactions
Exposure to poison ivy, poison oak, or poison sumac plants can cause an itchy, red rash at the base of contact. The rash may be in multiple areas, and it can be contained to either a small or large area, depending on its severity. Skin reactions to these plants are caused by the urushiol resin contained in the leaves, berries, twigs, branches, stems, and roots of these allergic plants. This oil penetrates the skin within minutes and causes an allergic reaction.
The best way to prevent these skin rashes, which can cause mild to severe discomfort, is to be able to recognize and avoid all contact with these plants.
- Poison ivy can be a low plant, vine, or high shrub. It has glossy green leaves in leaflets of three and produces clusters of small, whitish-green flowers in the spring that mature into white berries.
- Poison oak has three leaflets but has rounded lobes instead of pointed edges. This plant can be found in California and the southeast.
- Poison sumac grows in wet places in the eastern US and is usually in the form of small trees or small shrubs with 7-13 leaflets. The white berries help distinguish it from nonpoisonous sumacs.
Top 5 Ways to Reduce the Misery of Poison Ivy, Oak or Sumac Reactions
- Wet compresses or a cool bath may reduce swelling and itching.
- DO NOT apply strong chemicals, alcohols or other solvents. Nonprescription hydrocortisone creams are too weak to relieve the irritation. Topical anesthetics and antihistamines are not effective and may make symptoms worse.
- Do not pop blisters if they develop.
- Within 30 minutes of exposure, use over the counter products such as Zanfel Poison Ivy Wash, Tecnu Outdoor Skin Cleanser, and Ivy X skin cleanser to minimize reactions.
- Seek medical care with a board certified allergist if itching lasts more than a few days or is severe, if the rash covers a large area of skin, and/or if the rash involves the hands, face, eyes or gentitals.
Tip for managing poison ivy, oak, & sumac reactions:
Oils from these plants can “sneak” indoors on shoes and clothes, firewood, and pet fur. Be sure to remove shoes and clothing after exposure and/or contact with these plants and wash with ordinary detergent.
New Jersey Asthma & Allergy Friendly Summer Camps
- Camp Merry Heart- Easter Seals (Hackettstown, NJ)
- Camp TAG (The Allergy Gang) (Williamstown, NJ)
Pennsylvania Asthma & Allergy Friendly Summer Camps
- Camp AsthmaCadabra (Scranton, PA)
- Camp Chen-a-Wanda (Thomson, PA)
- Dragonfly Forest Camp (Poconos; Dingmans Ferry, PA)
Delaware Asthma & Allergy Friendly Summer Camps
- Asthma Camp (Newark, DE)
Maryland Asthma & Allergy Friendly Summer Camps
- Camp Superkids (Maryland Line, MD)
A Board-Certified Allergist Can Help
At The Asthma Center, our allergists and pediatric allergists help our patients and their parent prepare for summer camp by reviewing medications, avoidance measures and Action Plans.
The allergists, pediatric allergists, and asthma specialists at The Asthma Center treat patients in 9 convenient locations throughout the Delaware Valley including Philadelphia (Center City Philadelphia, Society Hill Philadelphia, Northeast Philadelphia), The Main Line – Montgomery County (Bala Cynwyd – Lower Merion PA), Bucks County (Langhorne PA), and South Jersey (Mt. Laurel NJ, Woodbury NJ, Hamilton NJ, Forked River NJ).
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
For interviews and tours of the Delaware Valley’s only National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com.
More Info
June 15, 2017. Father’s Day Allergy-Friendly Lawn & Grass Guide
Father’s Day Allergy-Friendly Lawn & Grass Guide
Check out The Asthma Center’s Father’s Day Allergy-Friendly Lawn & Grass Guide and keep allergies from mowing down your party or ruining your cookout. Father’s Day is almost here, and it’s time to give Dad a break!
Our board-certified allergists Lawn & Grass Guide is full of tips to help those will allergies, asthma, and sinus problem enjoy all the weekend fun and outdoor activities with Dad and the entire family.
Top 5 Ways to Keep Grass Pollen Out (of Eyes, Nose, and Home)
- Mow lawns regularly to cut down on grass pollination.
- Wear long sleeves, long pants, and wrap-around sun-glasses or glasses while mowing if lawn care is required.
- Be sure to shower & wash hair after mowing. Make sure you wash your face thoroughly including your eyebrows.
- Avoid mowing and limit your time outdoors during the early morning hours when most pollen is released.
- Beware of grass pollen “sneaking” into your home on pets and kids’ shoes/clothing, especially after playing outside in the grass, and on morning newspaper sleeves.
Mowing: Lawn Allergies & Cut Grass Smell
Mowing your lawn to reduce grass pollination, and limiting your exposure to grass pollen are both important steps in avoiding the misery of allergies.
In addition to grass pollen triggering allergy symptoms, many individuals experience typical allergy symptoms such as sneezing, itchy watery eyes, nasal congestion, and even wheezing when exposed to the smell of freshly cut grass. Allergic reactions triggered by the smell of freshly cut grass are likely from the nonpollen parts of the grass which also contain allergenic proteins or outdoor molds which have been stirred up by the mowing process. Concentrations of these allergy triggers dramatically escalate for a short period of time during and immediately after mowing. However, mowing lawns reduces grass pollination which can reduce symptoms over time. Following the above tips to reduce grass pollen will also help reduce exposure to grass allergenic proteins or outdoor molds when mowing the lawn.
Father’s Day Allergy-Friendly Grilling Guide
Father’s Day picnics and barbecues are common choices to “give Dad a break” which means family celebrations may include “firing up the grill.” Did you know that red meat allergy can be triggered by bites from the Lone Star Tick, a variety of tick that is active and prevalent in our region? Learn all the facts in our recent blog Allergic to Red Meat? Lone Star Ticks to Blame.
A Board-Certified Allergist Can Help
At The Asthma Center, our allergists and pediatric allergists help our patients manage their allergies by determining what local spring allergens cause symptoms. For example, with spring allergies, we identify which local grasses (including June, Kentucky Blue, Meadow Fescue, Orchard, Perennial Rye, Redtop, Sweet Vernal and Timothy) and trees trigger allergy symptoms by using minimally invasive in-house diagnostics, like allergy skin testing. Pairing these results with local knowledge of allergy triggers like pollen, ragweed and mold, our allergists develop personalized plans that treat not only the symptoms but also the cause of allergies. And because allergy symptoms often spike with pollen, we know exactly when to adjust allergy medication – providing more relief when conditions are bad and less medication every time else.
The allergists, pediatric allergists, and asthma specialists at The Asthma Center treat patients in 9 convenient locations throughout the Delaware Valley including Philadelphia (Center City Philadelphia, Society Hill Philadelphia, Northeast Philadelphia), The Main Line – Montgomery County (Bala Cynwyd – Lower Merion PA), Bucks County (Langhorne PA), and South Jersey (Mt. Laurel NJ, Woodbury NJ, Hamilton NJ, Forked River NJ).
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
For interviews and tours of the Delaware Valley’s only National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com.
More Info
May 22, 2017. Allergic to Red Meat? Lone Star Ticks to Blame
Allergic to Red Meat? Lone Star Ticks to Blame
With the warmer weather and spending more time outdoors, we are all more susceptible to tick bites. By now, most are familiar with Lyme disease from deer ticks. But did you know another tick variety prevalent in our area, the Lone Star tick, can trigger red meat allergy?
This red meat allergy is also known as alpha-gal allergy. Alpha-gal is a carbohydrate found in red meat including beef, pork, lamb and venison. Since 2009, Lone Star tick bites have been linked to the development of delayed allergic symptoms (usually 3-6 hours) following the ingestion of red meat. Individuals bitten by Lone Star ticks may develop allergy (IgE) antibodies to alpha-gal. Upon ingesting mammalian meat containing alpha-gal (red meat), delayed allergic symptoms can develop.
Red meat allergy is uncommon in the United States, and was only recently recognized in 2009. However, the increased population of Lone Star ticks in our region increases the threat of red meat allergy. An essential part of any food allergy treatment program is avoidance, and triggers can be particularly difficult to identify. This is particularly true with Lone Star tick bites and red meat allergy because the allergic reaction is often delayed, thereby “hiding” the true cause of the allergic reactions.
The Asthma Center Allergists have put together the following guides to help recognize the signs and symptoms of red meat allergy caused by Lone Star tick bites.
Lone Star Tick Bite Facts
- The Lone Star female adult tick has a distinctive white dot. The Lone Star adult male, on the other hand, has markings similar to those of a “deer tick.”
- Lone Star tick bites often cause an extremely itchy rash around the bite within 7 days. Note: Tick bites related to Lyme Disease and other illness by contrast, may also develop a rash that feel warm to the touch but generally are not itchy.
- Some individuals may be unaware that they have experienced a tick bite.
- Lone Star tick bites do not usually cause Lyme Disease; however, Lone Star ticks feed on warm blooded mammals which may have Lyme Disease and other tick-borne illnesses. In rare cases, the Lone Star tick can become a “carrier” of these illnesses.


Lone Star Tick Bites and Food Allergy Symptoms
After a Lone Star tick bite, the following food allergy symptoms can occur with the ingestion of red meat (including beef, pork, lamb or venison):
- Hives or skin rash
- Nausea, stomach cramps, indigestion, vomiting, diarrhea
- Stuffy/runny nose
- Sneezing
- Headaches
- Asthma
- Anaphylaxis (life-threatening allergic reaction)
Red Meat Allergy Diagnosis and Treatment
At The Asthma Center, our allergists and pediatric allergists help our patients manage their food allergies by first determining what foods cause symptoms. Commercially available allergy skin tests for red meat (beef, pork, and lamb) are usually negative, but skin tests to fresh meat may be positive. When a meat allergy is causing any of the above symptoms, and a Lone Star tick bite is suspected, a blood test can help diagnosis this condition. Many cases of what has previously been diagnosed as “idiopathic anaphylaxis (where the cause is unknown) may actually be cases of red meat allergy. The delayed reaction caused by red meat allergy (which can occur 3-6 hours after eating red meat) is often misleading since most allergic food reactions occur within one hour of ingestion of the culprit food.
Avoidance of foods that trigger symptoms is a key part of living with red meat food allergy. The Asthma Center allergists pair these results and any other testing results which may apply to an individual’s unique history and set of symptoms to identify specific triggers. The Asthma Center allergists also help our patients find relief of symptoms with antihistamines and corticosteroids, and prepare for anaphylaxis by carrying epinephrine auto-injector to reverse severe reactions to any unforeseen exposure or accidental ingestion of a triggering food.
Tips for Tick Bite Avoidance
No tick bite is a “good” tick bite.
With a greater than usual tick population predicted for our region, increases in Lyme Disease which is spread by the “deer tick” (black legged tick) are not the only concern. It has been widely reported that a small percentage of deer ticks may also carry the Powassan virus.
Avoid Tick bites:
- Use repellent that contains 20 percent or more DEET, picaridin, or IR3535 on exposed skin for protection that lasts several hours
- Walk in the center of trails and avoid wooded and grassy areas
- Wear long sleeves, long pants and thick socks
- Learn more about preventing tick bites from the Centers for Disease Control
If you are concerned about a tick bite or other rash, please see a medical professional.
The allergists, pediatric allergists, and asthma specialists at The Asthma Center treat patients in 9 convenient locations throughout the Delaware Valley including Philadelphia (Center City Philadelphia, Society Hill Philadelphia, Northeast Philadelphia), The Main Line – Montgomery County (Bala Cynwyd – Lower Merion PA), Bucks County (Langhorne PA), and South Jersey (Mt. Laurel NJ, Woodbury NJ, Hamilton NJ, Forked River NJ).
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
For interviews and tours of the Delaware Valley’s only National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com.
More Info

May 18, 2017. Yellow Smoke? It’s Pine Pollen!
Yellow Smoke: Pine Pollen Takes Over Delaware Valley
Despite the abundance of pine pollen in our air samples, pine pollen allergy is often ignored. “For individuals who today are sneezing, itching, have itchy watery eyes and/or other allergy & asthma symptoms, exposure to multiple aeroallergens—what’s in the air—especially pine pollen in our air matters now,” explains Dr. Marc F. Goldstein, board-certified allergist at The Asthma Center. “Pine pollen makes our region unique from an allergy perspective compared to other areas of the Northeastern U.S. where pine pollen is minimal, nonexistent, or other species are prevalent.”
Pine Pollen Unique to the Delaware Valley
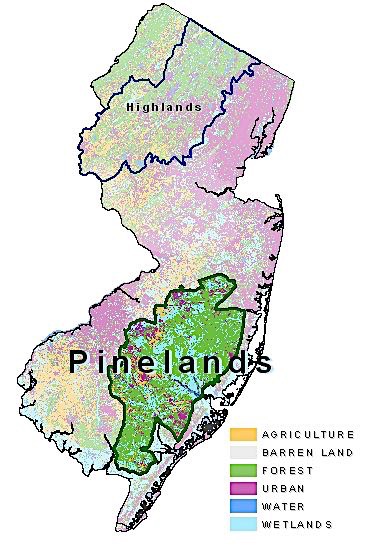
Within the heart of the Delaware Valley sits the 1.1 million acre (see map) protected open space known as the New Jersey Pinelands. Although there are over 110 different species of the pine family (Pinus), this protected area is home to the largest cluster of pitch pine, Pinus rigada (see picture below) on the United States (U.S.) Eastern coastline.
Dr. Donald Dvorin, board-certified allergist and the region’s official pollen counter, has been studying the tree pollen seasons in the Delaware Valley each spring for years. From the very beginning, he has observed notable pine pollen levels in both our Southern New Jersey and Philadelphia air samples. According to Dr. Dvorin, typically pine tree pollen appears in late May through the end of June.
Despite the abundance of pine pollen in air samples, pine pollen allergy is often ignored. Allergists both locally and nationally have for years felt that pine pollen is not a clinically relevant allergen, and many rarely test for pine pollen allergy. Some studies suggest that the prevalence of pine pollen allergy may range from 2%-10% of the population; however, there have been no studies that have firmly established the incidence of pine pollen allergy in the general allergic population.
Because of our region’s proximity to the Pinelands, the board-certified allergists continue to clinically recognize allergic symptoms at this time of year can be caused by pine pollen allergy. “We have included pine pollen in our allergy skin testing panel for years because we’re near the Pinelands and we know significant levels of pine pollen can be in the air,” explains Dr. Goldstein.
As seen in the picture above, pine trees can release large amounts of the yellow-colored pollen at a time. People often describe the effect as observing plumes of yellow smoke.
Why is Pine Pollen Ignored?
Pine pollen grains typically bear a waxy thick coat that surrounds its rather large size. Pine pollen grains can be 60 to 100 micrometers in diameter, large compared to other pollen grains (typical pollen grain size is approximately 10 micrometers). Doctors often believed that the size of pine pollen prevented its distribution by wind and through the air. However, studies and Dr. Dvorin’s own pollen counts have proven that this not the case. Despite its large size, pine pollen is capable of traveling great distances.
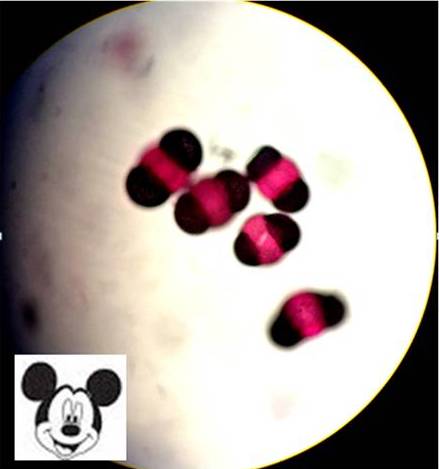
The pine pollen grain typically has 2 large air sacks that give it a “Mickey Mouse” appearance (see picture.) These air sacks reduce the pine pollen grain density and contribute to the pollen’s buoyancy, allowing it to travel long distances in the air. As an example, the center of the Pinelands is about 40 miles from Center City Philadelphia. Yet urban air samples from our Philadelphia, PA pollen collection station generally show the same relative volume of pine pollen grains as found in our suburban air samples from the Mount Laurel, NJ collection station which is 30 miles from the Pinelands. Thinking that the size of pine pollen grains were too large to enter the nasal and lung passages, many physicians (including allergists) did not consider pine pollen a relevant allergen. Evidence that it can be inhaled and provoke symptoms are found in cases reported in the medical literature as far back as 1921. Published results from limited investigation of pine pollen allergy have shown that pine pollen allergy does in fact cause allergic responses in the skin (positive allergy skin tests) and allergy responses on nose, eye, and lung challenges.
In addition to the limited reports of pine pollen-induced hay fever or bronchial asthma, there have been reports of allergies to ingested pine nuts (the seeds of pine trees) or from pine nuts found in pesto, sauces, salads, meatballs, cakes, candies and cookies. Interestingly enough, there is very little cross reactivity of pine nuts with other tree nuts. This is due to the fact that, evolutionarily, pine nuts are not from flowers as in the case of other tree nuts (like walnut, hazelnut, cashew, pistachios), but are contained within the pine cone—making them antigenically different from other tree nuts.
Another unusual manifestation of pine pollen sensitivity is in those who have “Christmas tree allergy.” This may be due to pine pollen being released from pine cones when cut trees are hydrated in the home causing nasal, eye, and chest symptoms during the holiday season.
Pine Pollen Allergies? Tips for Relief
Typically, pollen in the air tends to peak around early-morning, causing symptoms to be at their worst then. Luckily, there are a few ways to mitigate your worst allergy symptoms. Here are some best-practice tips for keeping your weekend allergy free:
- Wear long sleeves and long pants when mowing the grass
- Sleep with windows closed and drive with windows up
- Beware of tracking pollen into homes (kids, pets especially, newspaper sleeves, and on shorts and jackets)
- Shower and wash hair after extended outdoor exposure
- Wear wrap-around sunglasses or glasses outdoors to limit exposure of pollen to eyes
- Avoid wearing contact lenses, or switch to daily disposable contacts to avoid allergens building up on the lenses
- Wash hands and face frequently, including eyebrows
- Change pillowcases often
Board-Certified Allergists & Pediatric Allergists
The board-certified allergists at The Asthma Center are very much aware, therefore of the importance of pine pollen as an important spring allergen. Many patients who previously escaped diagnosis of seasonal pine pollen allergy was due to the fact that allergy skin testing to pine pollen was not performed or was not considered as a clinically significant allergen capable of provoking symptoms. If you would like to know if pine pollen allergy is playing a role in your symptoms, the allergists at The Asthma Center routinely test for pine pollen sensitivity and can effectively treat symptoms once identified—contact the office location near you to schedule an appointment!
Be sure to check back in for The Asthma Center’s Daily Pollen, Ragweed and Mold Spore Count, the Delaware Valley’s ONLY official pollen count station, certified by the National Allergy Bureau. Subscribe to receive our daily counts by email or check out some of our other blog posts to learn more about what is in the air, how it can affect you, and what you can do about it.
More Info
May 15, 2017. Food Allergy Awareness Week 2017: Oral Allergy Syndrome (OAS)
Food Allergy Awareness Week 2017: Oral Allergy Syndrome (OAS)
With allergies and asthma on the rise in the United States, education and awareness are critical to attaining proper treatment and care. This is particularly true regarding food allergies. This week (May 14-20, 2017), The Asthma Center joins Food Allergy Research and Education (FARE) in celebrating 20 years raising awareness on the seriousness of food allergies.
Itchy Mouth After Eating? Food Allergy & Pollen
Does your mouth, throat and/or lips become itchy after eating raw fruits and vegetables? Do you have pollen allergy? If you answered “yes” to both of these questions, you may suffer from a type of food allergy called Oral Allergy Syndrome (OAS). This syndrome is also known as Pollen-Food Allergy Syndrome (PFAS).
What Do I Need To Know About Oral Allergy Syndrome (OAS)?
- The most common symptoms of OAS include itching, tingling and/or mild swelling of the mouth, throat and/or lips. Less commonly, nausea and/or stomach upset. Reactions can be life-threatening, with systemic allergic reactions occurring in nearly 9% of individuals, with anaphylactic shock in 1.7% of those affected by OAS.
- Itching in OAS is caused by local allergic reactions triggered by contact of the lips, mouth and throat with allergenic proteins found in raw fruits and vegetables that are cross-reactive with allergenic proteins found in pollen to which an individual is allergic. Symptoms may also be caused by peanuts, tree nuts, spices and soybean.
- OAS most commonly has its onset in older children, teens and young adults who have eaten the suspect foods for many years with no allergic or other adverse reactions.
- Symptoms typically develop immediately after eating suspect foods and usually resolve within minutes of swallowing the foods. In rare cases, symptoms can develop up to one hour after eating. Symptoms are generally most severe during the related pollen season. Medical treatment is usually not necessary.
- Specific pollens have been associated with OAS symptoms triggered by specific foods. Examples include:
Birch pollen: apple, almond, carrot, celery, cherry, hazelnut, kiwi, peach, pear, plum.
Grass pollen: celery, melons, oranges, peaches, tomato.
Ragweed pollen: banana, cucumber, melons, sunflower seeds, zucchini.
What Should I Do If I Suffer from OAS?
- The best treatment is avoidance! Avoid foods which elicit OAS symptoms. This is particularly important in light of the low, but real, risk of anaphylaxis.
- Cooking foods thoroughly may prevent OAS symptoms by denaturing proteins in the foods and rendering them less recognizable to the immune system and, consequently, less likely to cause allergic reactions (e.g. most individuals can eat apple pie even though they can’t eat raw apples; for those with no history of milk allergy or lactose intolerance, a nice scoop of vanilla ice cream on top is recommended).
- Consultation with an Allergist is highly recommended to evaluate for pollen allergy and to define whether food-related symptoms are due to OAS, or true life-threatening food allergies. Treatment of pollen allergy with allergen immunotherapy (allergy shots) in those individuals with allergic rhinitis and/or asthma has been shown to be effective in reducing symptoms of OAS.
- Always carry an epinephrine auto-injector (e.g. EpiPen or AuviQ) to have immediately available to use in the event of an anaphylactic reaction.
So, beware! If you are allergic to tree, grass and/or weed pollen, you may be at risk for Oral Allergy Syndrome.
Board-Certified Allergists, Pediatric Allergists & Asthma Specialists
Effective treatment of food allergies and other related medical conditions first depends on a correct and proper diagnosis. Seeing a board-certified allergist is your first stop to healthy living with food allergies.
Our allergists, pediatric allergists, and asthma specialists treat patients in 9 convenient locations throughout the Delaware Valley including Philadelphia (Center City Philadelphia, Society Hill Philadelphia, Northeast Philadelphia), The Main Line – Montgomery County (Bala Cynwyd – Lower Merion PA), Bucks County (Langhorne PA), and South Jersey (Mt. Laurel NJ, Woodbury NJ, Hamilton NJ, Forked River NJ).
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease. For interviews and tours of the Delaware Valley’s only National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com.
More Info
May 11, 2017. Mother’s Day Allergy-Friendly Flowers Guide
Philadelphia, PA – May 11, 2017 – Rain or shine, Mother’s Day is around the corner. Flowers are synonymous with both Mother’s Day and allergies. Read The Asthma Center’s board-certified allergists’ Mother’s Day Allergy-Friendly Flowers Guide to keep your celebration “sneeze-free.” Happy Mother’s Day!
Allergy-Friendly Flowers
Individuals who have respiratory allergies may experience difficulty around flowers and other plants in indoor as well as outdoor garden environments. Fortunately, there are many flowers, shrubs, trees, and grasses that produce very little or no pollen and can be used in both indoor and/or outdoor environments. Fun Fact: Only male plant species produce the pollen that people react to, so that if you are able to purchase female plants you can be sure that they do not produce pollen.
For a less symptomatic weekend with Mom, try one of these allergy-friendly flowers more suited for allergy sufferers:
- Begonia
- Clematis
- Columbine
- Crocus
- Daffodil
- Geranium
- Hydrangea
- Iris
- Lily
- Periwinkle
- Rose
- Tulip
- Zinnia
Allergy Tips for Enjoying Flowers & Bouquets
The pollen from flowers used in arrangements is heavier than tree, grass and weed pollen. This means that usually it is less of a trigger for allergy and asthma symptoms, but it may still cause problems. Here is a set of allergy tips to keep in mind when giving or receiving flowers as a gift:

- Before you bring any ornamental flowers indoors, remove as much pollen as possible by removing the stamen. Wipe stems, leaves, and petals as needed.
- Resist the temptation of placing your nose directly in a bouquet of flowers or touching the flowers, since direct contact on the hands, other parts of the skin, eyes and nose may trigger allergy symptoms.
- The fragrance from some plants may also have a very significant irritant effect if you have respiratory allergies and/or asthma. Try to avoid particularly fragrant flowers.
- Reduce symptoms by avoiding the “worst offenders” such as chamomile, chrysanthemums, daisies, goldenrod, and sunflowers. Choose allergy-friendly flowers instead (See List Above.)
Dr. Goldstein on Allergy-Friendly Flowers
Our very-own allergist Dr. Marc Goldstein discusses allergy-friendly flowers and bouquets.
Board-Certified Allergists, Pediatric Allergists & Asthma Specialists
At The Asthma Center, our allergists and pediatric allergists help our patients manage their allergies by determining what local spring allergens cause symptoms. For example, with spring allergies, we identify which local trees, grasses, and flowers trigger allergy symptoms by using minimally invasive in-house diagnostics, like allergy skin testing. Pairing these results with local knowledge of allergy triggers like pollen, ragweed and mold, our allergists develop personalized plans that treat not only the symptoms but also the cause of allergies. And because allergy symptoms often spike with pollen, we know exactly when to adjust allergy medication – providing more relief when conditions are bad and less medication every time else.
Our allergists, pediatric allergists, and asthma specialists treat patients in 9 convenient locations throughout the Delaware Valley including Philadelphia (Center City Philadelphia, Society Hill Philadelphia, Northeast Philadelphia), The Main Line – Montgomery County (Bala Cynwyd – Lower Merion PA), Bucks County (Langhorne PA), and South Jersey (Mt. Laurel NJ, Woodbury NJ, Hamilton NJ, Forked River NJ).
Ask about our Special Spring Saturday Hours for New Patients (available in selected locations)!
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease. For interviews and tours of the Delaware Valley’s only National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com.
More Info













