Summer Camp for Kids with Allergies and Asthma: Blueprint for Fun
Summer Camp for Kids with Allergies and Asthma: Blueprint for Fun
It’s time for Summer Camp! The Asthma Center’s board-certified allergists have prepared the following guide, Summer Camp for Kids with Allergies and Asthma, to help parents and kids in the Delaware Valley get camp-ready for summer fun and making memories with friends.
Allergy & Asthma Action Plan
Preparation is the foundation of any summer camp experience, but this is especially true for children with allergies and asthma. No two children are alike, so pre-camp planning needs to be tailored to each child’s unique history and diagnoses. Our board-certified pediatric allergists meet with parents and children every year to help them create an appropriate Allergy & Asthma Action Plan in order to ensure a happy and safe summer camp experience for kids who may have:
- allergies to pollen, molds, and/or dust
- asthma
- food allergies and/or oral allergy syndrome
- bee sting allergies
- other insect sting allergies and reactions to insect bites
- poison Ivy, Oak, & Sumac reactions
The first step in creating an Asthma & Allergy Action Plan is identifying and listing your child’s triggers, symptoms and conditions. A written plan should cover not only current medication and allergies but also what instructions to follow in the event of an escalation of symptoms or an emergency.
Walking through an allergist-approved Action Plan with summer camp medical staff and camp leaders ensures that the camp staff understand how best to react in an emergency situation, and allows you as the parent to have confidence in the medical care available to your child while they are away from home. For example, if your child carries an epinephrine auto-injector (Epi-Pen, Jr; Auvi-Q), review your child’s Anaphylaxis Action Plan carefully with camp staff, and ask if which staff members are trained to administer epinephrine (and/or other emergency medical care.) Finally, it also can be useful to inquire how the camp has handled allergies, asthma, and reactions to foods or bee stings in the past.
Pre-Camp Medication Tip for Parents:
Summer is not the time to take a break from allergy and asthma medications. Visit your allergist well in advance to review medications. Before a child leaves for camp, make sure sufficient quantities of medications are available and check expiration dates.
Summer Camp for Kids with Allergies to Pollen, Molds, and/or Dust

For kids with allergies to pollen, molds, and/or dust, avoiding exposure to triggers that may cause allergy symptoms to flare can be challenging with outdoor activities while at summer camp. A board-certified pediatric allergist can identify a child’s specific allergy triggers through allergy skin testing, and provide a written Allergy Action Plan for both kids and camp staff. Ask what measures, if any, are followed to reduce allergen exposure. For example, are mold-inhibitors used to keep sleeping areas such as tents and cabins free of mold growth? What measures are used to keep dust exposure at a minimum?
Summer Camp Pollen and Mold Count Tip for Parents:
Ask if medical staff follow pollen, ragweed and mold spore counts for it’s geographic area. Knowing the daily pollen, ragweed, and mold spore counts can be invaluable in planning daily activities and following a child’s Allergy Action Plan (increasing or decreasing medications) and reducing the impact of exposure to a child’s allergy triggers. In the Delaware Valley, The Asthma Center’s official pollen, ragweed, and mold spore counts are available via email, on our website, and social media.
Summer Camp for Kids with Asthma
An Asthma Action Plan will include both a routine, day-to-day plan for kids with asthma and a written plan to follow in the case of an asthma flare. The Asthma Center specialists meet each summer with both parents and kids to discuss asthma action plans including the best ways to prevent asthma attacks while away from home and addressing any questions from children (or parents.) Talking with children who have asthma and answering any questions ahead of time may help “settle their nerves” so they can enjoy their summer experience.
Parents who are concerned about the capability of a specific camp in meeting their child’s asthma needs can also consult with their specialists regarding options, alternatives and “Asthma Camps.” (See list of local Asthma Camps at the end of this blog.)
Summer Camp Asthma Tip for Parents:
Be sure that camp staff know how to contact your child’s asthma specialist in the event of an emergency or asthma flare.
At The Asthma Center, one of our specialists is always on call – if your child needs help, a doctor who knows their medical history will be able to assist remotely.
Summer Camp for Kids with Food Allergies & Oral Allergy Syndrome

Food allergy symptoms can occur within several seconds or hours following food injection, although most reactions occur within the first 2 hours. The following symptoms can occur singly or in combination: Hives; swelling; eczema; itching of the mouth, throat, skin, palms, soles, or genitals; feeling of warmth; feeling of doom; vomiting; diarrhea; abdominal pain; cramping; nasal congestion; shortness of breath; chest tightness; cough; congestion (It is uncommon to see respiratory symptoms alone without gastrointestinal or skin symptoms.), dizziness, feeling faint, and passing out. Aside from the physical reactions, food allergies clearly affect the quality of life of affected individuals and their psychological welfare, especially of children. The “Big 8” (most common) triggers of food allergy are:
- milk
- eggs
- fish
- crustacean shellfish
- tree nuts
- peanuts
- wheat
- soybean.
Oral Allergy Syndrome is a type of food allergy which occurs in children (and adults) who have seasonal hayfever (allergy) symptoms and experience allergic symptoms in and around the mouth after eating certain foods including vegetables, nuts, seeds, and/or fresh fruits.
A board-certified allergist can help identify the specific triggers of both food allergies and/or oral allergy syndrome. Once a triggering food is identified, the best prevention is avoidance. However, for kids with food allergies, a Food Allergy Action Plan is essential for summer camp. A Food Allergy Action Plan, signed by a physician, should:
- outline step-by-step treatment recommendations for allergic reactions and/or anaphylaxis in the case of accidental exposure; and
- include emergency contact information.
To minimize stress while kids with food allergies are away from home at summer camp, provide multiple copies of your child’s Food Allergy Action Plan to the camp, and to your child, and discuss the plan with both camp staff and your child.
Summer Camp Food Allergy Tip for Parents:
If your child’s allergy requires an epinephrine auto-injector (EpiPen, Jr; Auvi-Q), and they are old enough to carry it with them, make sure they understand how to use it – and in what situation.
Stinging Stuff: Allergies to Bee Stings, Insects & Insect Bites

Insects such as bees, wasps, yellow jackets, hornets, and fire ants inject venom into the skin by “stinging” while other insects such as mosquitoes, fleas, black flies and ticks, use their saliva or bodies to produce reactions by “biting” and contact with skin. While most reactions to stinging and biting are mild to moderate, some adults and children experience sudden, severe and life-threatening reactions from stinging insects. Children who have been diagnosed with severe reactions to stinging insects should have an Anaphylaxis Action Plan, carry an epinephrine auto-injector, and wear an ID bracelet, anklet or necklace which identifies he/she as allergic to stinging insects.
Top 5 Ways to Reduce Risk of Insect Stings and Bites
- Wear shoes outside at all times.
- Wear white, green, tan, or khaki colors. Bright colored clothing is more likely to attract insects.
- Wear fitted clothing. Insects may become trapped in over-sized or loose, flowing clothes.
- Stay still when an insect is approaching. Never slap at an insect. Insects will not sting unless frightened or antagonized, so stay as calm and relaxed as possible.
- Avoid wearing scents, such as perfumes, hair sprays, and suntan lotion, which often attract insects. Keep foods and/or drinks covered while outside as these aromas may also attract insects.
If Attacked by Stinging Insects:
- Cover face with arms, and if possible, run and find shelter. Kids should find an adult or counselor immediately.
- Do not grab or squeeze any stinger attached to skin because this may cause more venom to inject into the wound.
- Remove a stinger and/or “venom sac” carefully by scraping the spot with your fingernail.
- Wash the area of the sting thoroughly with soap and water, and apply an antiseptic.
- Use cold compresses to the the site of sting for 15-20 minutes followed by Calamine lotion to reduce swelling and irritation.
- An oral antihistamine may be required to reduce itching.
Seek medical attention immediately if you notice signs of an allergic reaction such as widespread swelling, chest tightness, or dizziness.
Bee Sting Allergy Tip:
The Asthma Center’s board certified allergists recommend that any individuals who are sensitive to insect venom should be treated with venom injections, which has been proven to be effective in greater than 95% of individuals.
Lone Star Tick Advisory:
Did you know that red meat allergy can be triggered by bites from the Lone Star Tick, a variety of tick that is active and prevalent in our region? Learn all the facts in our recent blog Allergic to Red Meat? Lone Star Ticks to Blame.
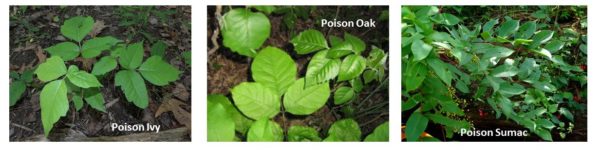
Avoid the Itch: Poison Ivy, Poison Oak, and Poison Sumac Reactions
Exposure to poison ivy, poison oak, or poison sumac plants can cause an itchy, red rash at the base of contact. The rash may be in multiple areas, and it can be contained to either a small or large area, depending on its severity. Skin reactions to these plants are caused by the urushiol resin contained in the leaves, berries, twigs, branches, stems, and roots of these allergic plants. This oil penetrates the skin within minutes and causes an allergic reaction.
The best way to prevent these skin rashes, which can cause mild to severe discomfort, is to be able to recognize and avoid all contact with these plants.
- Poison ivy can be a low plant, vine, or high shrub. It has glossy green leaves in leaflets of three and produces clusters of small, whitish-green flowers in the spring that mature into white berries.
- Poison oak has three leaflets but has rounded lobes instead of pointed edges. This plant can be found in California and the southeast.
- Poison sumac grows in wet places in the eastern US and is usually in the form of small trees or small shrubs with 7-13 leaflets. The white berries help distinguish it from nonpoisonous sumacs.
Top 5 Ways to Reduce the Misery of Poison Ivy, Oak or Sumac Reactions
- Wet compresses or a cool bath may reduce swelling and itching.
- DO NOT apply strong chemicals, alcohols or other solvents. Nonprescription hydrocortisone creams are too weak to relieve the irritation. Topical anesthetics and antihistamines are not effective and may make symptoms worse.
- Do not pop blisters if they develop.
- Within 30 minutes of exposure, use over the counter products such as Zanfel Poison Ivy Wash, Tecnu Outdoor Skin Cleanser, and Ivy X skin cleanser to minimize reactions.
- Seek medical care with a board certified allergist if itching lasts more than a few days or is severe, if the rash covers a large area of skin, and/or if the rash involves the hands, face, eyes or gentitals.
Tip for managing poison ivy, oak, & sumac reactions:
Oils from these plants can “sneak” indoors on shoes and clothes, firewood, and pet fur. Be sure to remove shoes and clothing after exposure and/or contact with these plants and wash with ordinary detergent.
New Jersey Asthma & Allergy Friendly Summer Camps
- Camp Merry Heart- Easter Seals (Hackettstown, NJ)
- Camp TAG (The Allergy Gang) (Williamstown, NJ)
Pennsylvania Asthma & Allergy Friendly Summer Camps
- Camp AsthmaCadabra (Scranton, PA)
- Camp Chen-a-Wanda (Thomson, PA)
- Dragonfly Forest Camp (Poconos; Dingmans Ferry, PA)
Delaware Asthma & Allergy Friendly Summer Camps
- Asthma Camp (Newark, DE)
Maryland Asthma & Allergy Friendly Summer Camps
- Camp Superkids (Maryland Line, MD)
A Board-Certified Allergist Can Help
At The Asthma Center, our allergists and pediatric allergists help our patients and their parent prepare for summer camp by reviewing medications, avoidance measures and Action Plans.
The allergists, pediatric allergists, and asthma specialists at The Asthma Center treat patients in 9 convenient locations throughout the Delaware Valley including Philadelphia (Center City Philadelphia, Society Hill Philadelphia, Northeast Philadelphia), The Main Line – Montgomery County (Bala Cynwyd – Lower Merion PA), Bucks County (Langhorne PA), and South Jersey (Mt. Laurel NJ, Woodbury NJ, Hamilton NJ, Forked River NJ).
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
For interviews and tours of the Delaware Valley’s only National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com.
Recent
Popular