Eye Allergies
People with eye allergies typically have symptoms that include:
- Itchy watery eyes
- Eyelid problems
- Dark circles around eyes
- Dry eyes
- Reactions to Contacts
Let us help allow you to see and look better!
Eye Anatomy: What Do Eye Allergies Actually Effect?
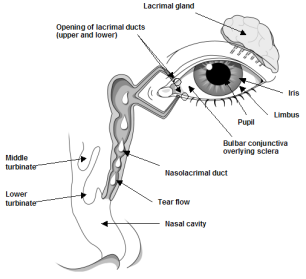
The eye is commonly involved in allergic reactions. The conjunctiva is the part of the eye that is most frequently affected during common allergic reactions involving airborne allergens. The conjunctiva consists of a clear membrane covering the white of the eye and the inside of the eyelid. It begins at the eyelid edge and covers the inside of the eyelid, including most of the white of the eye (sclera) up to the limbus. The limbus is the point where the conjunctiva ends and the cornea begins. The cornea is the most outer portion of the eye, and it is made out of a tough transparent tissue that is needed for vision. For a complete view of the eye anatomy, see Figure above. The conjunctiva is loose tissue, rich in fluids, blood vessels and cells. Some of the cells like mast cells are rich in chemical mediators (histamines) involved in allergic reactions. Bound to the mast cell surface are hundreds of thousands of IgE antibodies which can attach to allergens such as pollen, dust mite and animal dander. When airborne allergens contact the conjunctiva, they can attach to IgE antibodies on the mast cell surface, triggering an allergic reaction in the eye. Once mediators are released from mast cells, the conjunctiva blood vessels respond by opening and leaking fluids. The eye becomes red, inflamed, swollen and very itchy.
Allergic conditions of the eyes or tissue around the eyes include the following:
- Allergic conjunctivitis (seasonal or perennial)
- Atopic keratoconjunctivitis
- Vernal keratoconjunctivitis
- Giant papillary conjunctivitis
- Allergic conditions involving the eyelid include contact dermatitis and atopic dermatitis
Allergic Conjunctivitis: Eye Allergies
Allergic conjunctivitis is a common allergic problem involving the conjunctiva of the eyes. It is most frequently associated with symptoms of itchy watery eyes often occurring during the allergy seasons. Repeatedly rubbing the eyes perpetuates the itchy feeling and creates a repetitive cycle of infection.
Allergic conjunctivitis may be seasonal, affecting you based upon changing concentrations of seasonal pollen. Symptoms may also be perennial when exposure to allergens such as dust mites, indoor molds or pet dander is year round. Symptoms may also be episodic, for example after occasional exposure to a pet.
Seasonal allergic conjunctivitis is the most common allergic disease involving the eye. Eye allergies can be severe and quite intolerable but not dangerous since they do not cause any permanent damage to the eye. The disease usually is self limiting with avoidance of the allergen. Seasonal allergic conjunctivitis occurs more frequently than perennial allergic conjunctivitis. Symptoms typically occur in spring and fall depending on your specific sensitivities and the time and extent of pollen exposure.
Perennial allergic conjunctivitis typically results from exposure to dust mites, animal dander, and/or mold or other allergens that are present year round in home or work environments. Because of constant exposure to these allergens, symptoms are year round and similar to the symptoms of the seasonal condition. However, they may wax and wane depending on indoor allergen concentrations.
If you suffer from eye allergies, you may develop dark discoloration or circles below your eyes often called “allergic shiners.” You may complain of fullness in your eyes or perhaps a burning sensation. The eyes often tear and may become swollen or even swell shut in severe cases. Your eyes may be red or not even look that bad even though the itching is quite severe. You may complain of intolerance to bright lights (photophobia) or occasionally have blurred vision. When symptoms are severe, the need to rub your eyes may become overwhelming because of the intense itching.
Non-Allergic Eye Conditions
Non-Allergic conditions need to be considered and ruled out before final diagnosis of allergic conjunctivitis is made. Among these considerations are:
- Dry eyes which can cause red itch or burning sensation in the eye as if there is a foreign particle present (and watery eyes as overcompensation for dryness)
- Presence of a foreign body/particle
- Overuse of eye medications (topical decongestants used to “get the red out”) can cause red, irritated eyes even after all allergic or other symptoms have resolved; in this case, the treatment actually causes the disease
- Cosmetic or other contact allergy of the eyelids
- Contact lens related problems
- Medication induced conjunctivitis
- Work environment and hobbies-nonspecific air pollution from work or hobbies can cause irritated, red, watery, burning or stinging eyes
- Atopic dermatitis
- Eye or Eyelid Infections: Eye infections may be difficult to exclude early in the development of eye symptoms since they may be similar to that of allergy. Eye infections usually begin in one eye at a time, while allergy usually affects both eyes at the same time. The discharge from an infected eye may begin as clear but often becomes cloudy or discolored with time. In contrast allergic conjunctivitis is always associated with a clear discharge. Eye infections may be associated with swelling or tenderness of the small lymph nodes in front of the ear while this is not observed in allergic conjunctivitis.
Common Types and Symptoms of Conjunctivitis
|
Allergic |
Viral |
Bacterial |
|
|
Primary Complaints |
Itching, often severe |
Burning, irritation, discomfort |
Irritation |
|
Tearing |
Moderate |
Profuse |
Moderate |
|
Discharge |
Minimal, pinkish or milky |
Minimal |
Profuse, whitish purulent |
|
Redness |
Generalized |
Generalized |
Generalized |
|
Other Findings |
Nasal and/or chest symptoms |
Occasional sore throat and fever |
Occasional lid swelling |
Treatments for Eye Allergies & Eye Itching
Itching and tearing may cause you great distress, interfering with your ability to read, concentrate, work, attend school or even sleep. If you experience these problems, the following treatments are available for eye allergies:
- HEPA filters can limit exposure to airborne allergens
- Encasement of pillow and mattress may be used for dust mite allergy control
- A cold compress over the eyes can give immediate but temporary relief of symptoms
- When environmental controls prove inadequate in the management of symptoms the following medications may help:
- Oral antihistamines are often helpful but not always adequate for relief of symptoms
- The use of topical antihistamines or mast cell inhibitors may be effective
- Dual acting antihistamine and mast cell stabilizers are a good initial choice.
- In severe cases, combinations of medications including adding a topical nonsteroidal anti-inflammatory drug (NSAID) or temporary use of topical corticosteroids may be necessary.
- Rarely oral corticosteroids are used for a short period when symptoms are extraordinarily severe. Nasal corticosteroids are often helpful in the chronic treatment of eye allergies.
- If you have persistent or troublesome symptoms and continuing allergen exposure, allergy injection therapy or allergy shots should be considered to lower your sensitivity to the offending allergen
Atopic Keratoconjunctivitis
Atopic keratoconjunctivitis is a chronic inflammatory condition that affects both the conjunctiva and the eyelids. It is associated with atopic dermatitis, a condition characterized by dry, itchy easily irritated skin. Atopic dermatitis generally consists of eczema of the skin just above the forearm, on the back of the legs, hands, face and neck. This skin condition often begins in childhood and improves or resolves as you age. However, it is possible to have this condition into adulthood. Approximately 3% of the population has atopic dermatitis and only a minority of these individuals has associated allergic eye conditions such as atopic keratoconjunctivitis. If you suffer from atopic keratoconjunctivitis, you may suffer from severe itching, particularly of the eye and the skin over the eye. Unlike allergic conjunctivitis, the skin around your eyes may become dry, scaly, or reddened. The skin in this area may have barely visible microwrinkles, be thickened or have a slight increase in pigmentation from constant rubbing. Your lid margins may show loss of eyelashes. The underside of your upper lid may have islands of tissue (papillary hypertrophy) which may be irritated by contact lenses or may irritate the cornea. This complication is an important medical problem since it may result in damage to your vision if neglected. Symptoms of atopic keratoconjunctivitis may be seasonal perennial or both.
Vernal Conjunctivitis
Vernal conjunctivitis is an inflammatory eye condition that affects the conjunctiva and eyelids. The inflammation of the conjunctiva is chronic, severe and persistent. It affects both eyes and worsens from seasonal flares after exposure to an allergen. This condition usually begins in childhood and resolves around puberty, but it may also continue into adulthood.
If you suffer from vernal conjunctivitis, you may suffer from severe light sensitivity (photophobia) and itching. You may also complain of droopy eyelids, eyelid spasms and a sensation of something stuck in your eye. Your eyelid skin and margins may be normal. Often the mucosa aof the underside of the upper lid is heaped into giant bumps of mucosal tissue referred to as cobblestones or papillae. Unlike allergic conjunctivitis in which the discharge is clear and very liquidy, you will often have a thick, stick string-like mucous discharge that may need to be removed manually from time to time.
Diagnosis
Diagnosis of vernal conjunctivitis is based on the presentation of typical symptoms. You may have an allergy history or a family history of allergy. Identification and avoidance of relevant allergen(s) is extremely important. Allergy skin testing is the most sensitive method to determine potential sensitivity to particular allergens.
Treatment for These Types
- Environmental controls for environmental allergens at home, school, or in the work environment identified as triggering symptoms.
- When environmental allergen controls prove inadequate in the management of symptoms, the following medications may help:
- Topical antihistamines, decongestants and mast cell stabilizers or dual acting mast cell stabilizers and antihistamines are helpful, but they may take some time for optimal effect.
- In severe cases, a burst of oral corticosteroids or frequent application of topical corticosteroids is needed to relieve unbearable symptoms. Prolonged use of corticosteroids should be avoided because of their association with the complication of glaucoma and/or cataracts.
- Topical cyclosporine A may be useful in severe cases.
- Complication of corneal ulceration may require a combination of antibiotics, corticosteroid ointment and a gauze pressure dressing over the eye.
- Immunotherapy (allergy shots) should be considered to lower your sensitivity to known allergens.
Giant Papillary Conjunctivitis: Contact Lenses
Giant papillary conjunctivitis is a chronic inflammatory condition affecting the mucous membranes of the upper eyelids. It is most often caused by soft contact lenses, but it can occur with any type of lens, ocular prosthesis, or even exposed sutures.
If you suffer from giant papillary conjunctivitis, you may suffer from itchy eyes following removal of your contact lenses, irritation, redness, burning, mucous discharge, light sensitivity (photophobia) and increasing contact lens intolerance. These symptoms may begin months to years following your initial use of contact lenses. Sever symptoms such as blurring of vision can occur due to movement of your lenses secondary to the presence of giant cobblestones of mucosal tissue beneath the eyelid or from debris deposited on the lens during the underlying inflammatory process. This condition many occur more frequently if you have underlying allergies.
Diagnosis
Diagnosis of giant papillary conjunctivitis is primarily based on removal of contact lenses to differentiate between this condition and atopic keratoconjunctivitis.
Treatment for This Type
- Reduce contact lens use or discontinue lens use.
- Topical mast cell stabilizers such as cromolyn sodium and dual acting topical ophthalmic medication many be helpful
- Topical corticosteroids are effective in controlling more difficult symptoms
- When symptoms clear up, it may be possible to resume contact lens use if you switch to an alternative lens type along with the use of preventative medication
Eyelid Allergies: Swelling/Itching
Allergic reactions can also cause problems in the eyelid skin producing swelling, itching and/or redness of the lids. Allergic contact dermatitis to a chemical and/or eczema commonly cause problems in the eyelids as isolated skin problems or as part of a more generalized skin condition. Complete evaluation including allergy tests (patch testing and allergy skin testing) and blood work are often helpful in identifying the culprit(s). We have developed several evaluation and treatment strategies to limit and/or resovle these problems.












