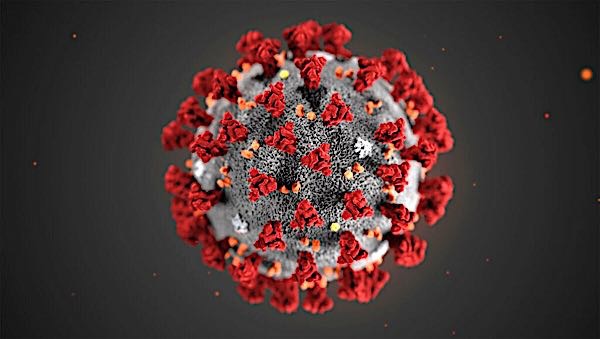
Allergic Reactions and The Coronavirus COVID-19 Vaccine: Is It Safe If I Have Severe Allergies?
By Dr. Marc F. Goldstein, Board-Certified Allergist at The Asthma Center (Philadelphia PA, Mt. Laurel NJ)
As the coronavirus (COVID-19) pandemic continues, there has been significant progress on the development of a COVID-19 vaccine. Will the coronavirus vaccines be safe to take for people with severe allergies (like peanut allergies, egg allergies or other food allergens)?
Do People Who Get The Coronavirus (COVID-19) Vaccine Get Allergic Reactions?
In the United Kingdom, there were two reported cases of severe allergic reactions occurring during the first day of public vaccination in the United Kingdom which have set off a flurry of questions about the safety of coronavirus (COVID-19) vaccines in individuals with a history of allergic reactions. The two individuals who suffered allergic reactions had a history of significant allergies (the nature of their allergic reactions and triggers have not been reported). The two patients recovered after treatment which may have included use of epinephrine.
How Common Is An Allergic Reaction to The Coronavirus (COVID-19) Vaccine?
Allergic reactions to vaccines, including a severe life-threatening anaphylactic reaction to a vaccine, are anticipated with any vaccine just as with drugs, but they are rare events. From large epidemiologic studies, anaphylaxis after vaccination occurs at a rate of 1.31 cases for every one million vaccine doses given. During the late stage clinical trials of the Pfizer/BioNTech COVID-19 vaccine clinical trials, there were 42,000 patients who received the vaccine administered in two doses and the allergic reaction rate was 0.63% in those who received the vaccine compared to 0.51% in those who received placebo. This difference was not statistically significant. This means that just about as many people had reactions to the placebo as had reactions to the vaccine. The severity and the nature of the reactions have not yet been reported. Patients who had a history of severe allergic reactions notably were excluded from participating in the clinical trial. People with common environmental allergies were not excluded from the study. Patients with common food allergies were also not excluded from the study because there is no trace of eggs, peanuts, tree nuts or other food protein in the vaccine.
Is It Safe To Get The COVID-19 Vaccine If I Have Severe Allergies?
As a consequence to the two reported cases of allergic reactions to the COVID-19 mRNA vaccine in United Kingdom, the United Kingdom Medical and Healthcare Products Regulatory Agency which sanctioned the use of the vaccine under emergency authorization in the UK, came out with a statement which said that people with a history of allergic reactions (significant reactions to vaccines, medicines, and foods) or a history of near fatal allergic reactions (anaphylaxis) should not receive the vaccine. This prohibitory precaution may, however, be an overreaction to the true risk of allergic reactions to the COVID-19 vaccines in the general public or to people who have had prior allergic reactions to medication and/or vaccines or have a history of anaphylaxis.
What Causes The Allergic Reaction in The COVID-19 Vaccine?
In general, allergic reactions to vaccines most commonly have been attributed to additional inactive components within vaccines like gelatin, egg protein, thimerosal, formaldehyde, possibly latex found in the rubber stoppers of vaccine bottles, and other possible excipients (inactive substances that serve as a vehicle or medium for an active substance like coloring agents, preservative, and fillers). Fatalities to vaccines have rarely been reported. The unique Pfizer vaccine has nucleoside modified messenger RNA genetic material which in itself is unlikely to produce an allergic reaction due to its size and structure. The messenger RNA is packaged in a lipid nanoparticle which holds the messenger RNA along with excipients including polyethylene glycol, sucrose, and a variety of salts. The lipid nanoparticle and salts are unlikely also to cause allergic responses in as much as these materials or similar materials are found naturally in the body and do not cause allergic reactions. Polyethylene glycol on the other hand has on occasion been reported as a cause of allergic reactions in some individuals.
How And Where Should I Get The COVID-19 Vaccine Safely If I Have Severe Allergies To Eggs or Peanuts or Other Allergens?
The COVID-19 vaccine, like all other vaccines, should be administered in a facility that can treat an allergic reaction if it occurs and as a precaution, the patient should routinely wait 20 to 30 minutes after vaccine administration in such a facility. Despite the United Kingdom statement, there may not be enough data at this point to justify the exclusion of patients who have a history of allergic reactions to foods, drugs, environmental allergens, or other vaccines, from COVID-19 vaccination. In fact, the FDA, after approving the Pfizer vaccine for emergency use, stated that the Pfizer coronavirus vaccine appears to be safe for people with food or environmental allergies. The only allergic warning is limited to a prior allergic reaction to the vaccine itself and/or an allergic reaction to a vaccine component. This warning is consistent with allergic warnings for other vaccines.
Patients who have a history of allergic reactions should inform their providers before getting vaccinated and they should receive the vaccine at a place where they can be observed for any adverse reaction for at least 20 minutes after the vaccine is administered. The facility should also have the capability of treating a severe allergic reaction. Though continued surveillance of adverse reactions, including allergic reactions, will be essential during the rollout of the new COVID-19 vaccines, based on the current available data, individuals with a history of allergic reactions should still consider taking the COVID-19 vaccine. However, anyone who has specific allergy concerns regarding the vaccine should speak with a knowledgeable board certified allergist.
Copyright (c) 2020
No reprints without written approval from Allergic Disease Associates, PC (The Asthma Center)
Recent
Popular