Uncategorized

July 7, 2020. Taking the Pain Out of Coronavirus Testing (PCR Test)
by Marc Goldstein, MD, Board-Certified Doctor at The Asthma Center
For those suspected of having COVID-19, a potentially painful nasopharyngeal swab collection (PCR assay for genetic viral material) is usually done to confirm the presence of the SARS-CoV2 coronavirus in the upper respiratory tract. This type of coronavirus test can be less painful with careful planning and proper pre-medication before getting tested.
How Does Coronavirus Testing (PCR Swab) Work?
The testing procedure itself uses a swab covered with an absorbent material that is pushed through the nose about 3 inches to the back of the throat. The swab is then twirled around for about 15 seconds and then withdraw. A helpful video about how to use the swab technique for coronavirus testing is published by the New England Journal of Medicine available here
Since the nose is not used to having any object placed inside, most people find this to be psychologically unnerving and physically a very uncomfortable process. In fact, if you do not experience some level of discomfort during the procedure, the test probably was not done correctly leading to unreliable results.
Is Coronavirus Testing (PCR) Painful?
Several different sensations can be experienced during PCR testing for coronavirus. People have reported transient pain, deep burning inside the nose, gagging when the back of the throat is touched, sneezing, coughing and tearing due to the triggering of a nasal lacrimal reflex. If you happen to have a significant septal deviation or have blocked nasal passages due to allergies, cold-like symptoms and or nasal polyps, it may be particularly challenging to pass the nasal swab to the back of the throat.
How Can I Make Coronavirus Test (PRC) Less Pain in My Nose?
One technique that may make the process easier is to simply apply an over the counter nasal decongestant (0.05% oxymetazoline, brand name Afrin) inside the nose 30 to 60 minutes prior to the procedure. One drop to each nostril applied while lying down is usually enough to decongest the nose so that when the swab is passed, the nasal airway is maximally opened. This can prevent the swab pushing up against the walls of the nasal passageway causing pain and sometimes bleeding. By the time the swab is collected and the coronavirus test is performed, there is very little residual oxymetazoline left in the airway to affect the viability of the virus or have an effect on the assay. In addition, sneezing, coughing and tearing may be prevented or lessened with taking an antihistamine 30-60 minutes before the test.
Making the process of collecting nasal secretions via a nasopharyngeal swab easier for the patient may increase testing acceptability and allow for better quality specimens for testing.
Telemedicine For Patients
The Asthma Center is available to provide the care you need during the coronavirus outbreak. While our offices are still open for in-person visits, our board-certified allergy and asthma doctors will also be available for telemedicine appointments for patients. Please learn more here or by calling The Asthma Center at 215-569-1111 (in Pennsylvania) or 856-316-0300 (in New Jersey).
The information contained in this article is the sole property of The Asthma Center and may not be repurposed for other use without permission from The Asthma Center.
More Info
April 12, 2020. Coronavirus vs Asthma: How to Tell The Difference?
by Marc Goldstein, MD, Board-Certified Allergist at The Asthma Center
Do I Have Greater Risk for Getting Coronavirus If I Have Asthma?
In a time when asthma symptoms may be flaring due to weather changes and seasonal spring pollens, people with asthma may worry whether their asthma may put them at risk for getting coronavirus (COVID-19). It can be confusing because both asthma and coronavirus share symptoms of cough and shortness of breath. The good news that the chance of getting coronavirus for anyone with asthma is really no different than for someone without asthma. Getting coronavirus comes down to an individual’s exposure to suspected or confirmed cases of coronavirus or to symptomatic carrier of SARS-CoV-2 virus (the virus that causes the COVID-19 infection). Therefore, to reduce your risk of getting coronavirus whether you have asthma or not, practice the social distancing, hand washing, mask and glove protection, and surface disinfection that has been promoted by the CDC and public health and infectious disease experts (see more here).
What If I Have Asthma and Coronavirus?
Though asthma does not in itself put you at greater risk to contract coronavirus, those individuals with some forms of asthma may be at risk for complications and may get sicker from coronavirus. The Surgeon General of the United States, recently brought this to the attention of the American public. However, according to the CDC, this concern applies only to individuals with persistent moderate to severe asthma though there is no published data that actually supports this assertion at this time. Fortunately, the vast majority of individuals with asthma have intermittent asthma meaning they have infrequent symptoms and use a rescue inhaler less than 2x/week not including preventative use before exercise. Individuals with moderate persistent asthma are usually on a maintenance inhaler which contains moderate to high doses of inhaled steroids with or without long acting bronchodilators. Individuals with severe persistent asthma are on higher doses of inhaled steroids with or without biologic therapy ( Xolair, Nucala, Dupixent, Fasenra, Cinquair) and have significant limitations in lung function.
Since coronavirus can infect your respiratory tract (nose, throat, lungs), the COVID-19 respiratory virus, like other respiratory viruses like influenza, can precipitate an asthma attack and possibly lead to a viral pneumonia and in the worse case acute respiratory failure from ARDS (acute respiratory distress syndrome.).
How To Tell If My Cough is From Coronavirus or Asthma?
Unfortunately, people can have both asthma and coronavirus. Here are a set of tips to help understand the symptoms that you feel.
- Typical coronavirus symptoms include fever (temperature over 100.4 degrees) , joint or muscle aches and pain, as well as dry cough and significant shortness of breath. Asthma usually does not cause fever unless accompanied by a respiratory infection and usually does not cause the muscle and joint symptoms typical of coronavirus.
- Individuals with asthma often wheeze and feel tightness in the chest. These symptoms are less frequent with COVID -19.
- For those who have had asthma for years and have gone through flares, their symptoms are very familiar. If some of your chest symptoms are atypical for you and you have fever as well, it is worth speaking with your Asthma Center physician as to whether you have COVID 1- 19 and be tested as well as getting your asthma under control. COVID-19 can exacerbate your asthma and it is important to remember andindividual with asthma can experience symptoms from both an asthma flare and from COVID-19.
- Seasonal asthma during the spring may be related to tree and grass pollen, and may also be coupled with allergies in the nose, throat, eyes and ears. With those individuals having typical allergy symptoms in the context of cough and even shortness of breath without fever, the latter symptoms are most likely allergy and asthma and not coronavirus. Coronavirus rarely causes sneezing, runny or stuffy nose. Both conditions can cause loss of smell.
What Is The Most Important Thing To Know If You Have Asthma During Coronavirus?
The most important thing an asthmatic individual should do at this time is make sure their asthma is well controlled and that they follow coronavirus precautions to prevent getting infected. Having your asthma controlled well helps keep your lung function at a higher level allowing you a better chance of getting through coronavirus in your lungs.
Coronavirus decreases the functioning of your lungs. For example, a well-controlled asthmatic with 90% of lung function (without coronavirus) will have an easier time of handling a coronavirus infection in the lungs that decrease lung function to 60%. Compare this to a poorly-controlled asthmatic who starts at 70% of lung function and drops to 40% with a coronavirus pneumonia. Starting at a higher lung function by well-controlling and treating your asthma, will help you better fight a coronavirus infection.
Seeing your health care provider at this time (either through telemedicine or in office) is critical for you to improve your chances to beat coronavirus.
What Are Tips For Asthma Sufferers During Coronavirus?
It is important also that your asthma symptoms are well controlled so that those around you do not misconstrue coughing as a symptom of coronavirus when in fact the cough is non infectious from asthma. The following recommendations are important for those with asthma particularly those with persistent moderate to severe asthma. Following these added precautions will decrease your chance of getting coronavirus and having your asthma flare with coronavirus.
- Keep your asthma well controlled with proper medication and using inhalers properly. This may require seeing your Asthma Center provider in-person or through telemedicine.
- Keep your nose and eyes clear of allergies to prevent allergies from triggering your asthma.
- Do not stop your current asthma medicines or change your medication without speaking with your Asthma Center allergist. Do not stop your inhaled steroid medication. Some individuals stop their inhaled steroids because they are concerned they may suppress their immune system. This is not the case and inhaled steroids are important therapies to reduce asthma symptoms and prevent attacks.
- Make sure you have at least a 30 supply of your current and backup asthma medication on hand in case you need to stay home for a long time.
- Avoid your asthma triggers, which may mean you should only go outside when pollen exposure is least like in the late afternoon or evening or after a rain shower.
- If you are living with cats and or dogs which you are allergic too, your asthma may flare due to spending more time spent indoors and exposure to animal dander. Remove your pets from your bedroom, limit physical contact and run a HEPA filter in your bedroom and other rooms of your home where you spend time.
- During this time, it is natural to feel stressed and anxious which may also trigger your asthma. If you find yourself in this situation family, friends and community leaders may be of support as well as methods of behavioral relaxation which you may find online. For some, connecting with a therapist through telemedicine may also be beneficial.
- If possible, have someone without asthma do the disinfecting and cleaning of surfaces since many cleaning produces may induce asthma. Make sure you are not in the room when disinfectants are applied. Make sure the following surfaces remain clean and disinfected: phone remotes, tables, doorknobs, lights switches, counter tops, handles, desks, keyboards, toilets, faucets and sinks.
- There is some concern that nebulizers if used by people infected with coronavirus may aerosolize viral droplets allowing the virus to stay in the air longer and increasing the risk of infecting others. Some hospitals have abandoned the use of nebulizers for this reason. At home, if you use a nebulizer, it may be of benefit to use it isolated from other household members and run a HEPA filter in the room as well to decrease the risk of infecting other people in your household.
- If chest symptoms develop and do not respond to initial backup medications and/or you have a fever with your chest symptoms, call your healthcare provider. The bottom line for people with asthma during the COVID-19 pandemic is to maintain control of your asthma with proper medication under the guidance of your health care provider. Maintaining social distancing, hand washing, wearing a protective mask and gloves outside your home and surface disinfection,in addition to staying out of the emergency room for asthma flares will improve your chances to get through this outbreak.
The bottom line for people with asthma during the COVID-19 pandemic is maintain control of your asthma with proper medication under the guidance of the allergy and asthma specialist at The Asthma
Center. Maintaining social distancing, hand washing, wearing protective mask and gloves outside your home, surface disinfection, in addition to staying out of the emergency for asthma flares will maximize
your chance of safely getting you through this outbreak.
Telemedicine For Patients
The Asthma Center is available to provide the care you need during the coronavirus outbreak. While our offices are still open for in-person visits, our board-certified allergy and asthma doctors will also be available for telemedicine appointments for patients. Please learn more here or by calling The Asthma Center at 215-569-1111 (in Pennsylvania) or 856-316-0300 (in New Jersey).
The information contained in this article is the sole property of The Asthma Center and may not be repurposed for other use without permission from The Asthma Center.
More Info
March 11, 2020. Coronavirus, Common Cold or Allergies?
The recent outbreak of coronavirus has crossed paths with the start of the spring pollen allergy season and the end of “cold season.” Since there is overlap in symptoms, it is important to categorize and distinguish amongst these problems to benefit from the most appropriate care. The following chart lists common symptoms of each.
|
|
Symptoms |
Onset |
Typical Duration |
|
Colds |
Runny nose with yellow discharge Sneezing Weakness and fatigue |
Symptoms develop within 1-3 days of exposure to the cold virus |
5-10 days |
|
Allergies |
Congestion Runny nose with thin, watery discharge Sneezing Wheezing Coughing Itchy nose, throat, eyes, and ears (nose & chest secretions are not contagious) |
Symptoms begin almost immediately after exposure to specific allergen(s). If seasonal allergies, symptoms occur at the same time every year. If perennial allergies, symptoms are present year-round |
Symptoms last as long as you are exposed to the allergen. If that allergen is present year-round, symptoms may be chronic |
|
Coronavirus (with COVID-19) |
Fever Shortness of Breath Cough (nose & chest secretions are contagious) |
Symptoms develop up to two weeks after exposure to the virus. The virus is thought to spread mainly through close contact between people. |
Variable: days to weeks |
There is no curative treatment for these illnesses, but proper care can help relieve symptoms and reduce risk of developing complications. Speak to your healthcare professional about options for relief.
Allergies vs Coronavirus Symptoms
Seasonal allergies can result in a range of symptoms including congestion, runny nose (thin discharge), sneezing, wheezing, cough, and itchy nose, throat, and eyes. These symptoms are most common in Spring and Fall upon exposure to seasonal pollens, and should not be confused with coronavirus. If you have a fever as well, you are likely not experiencing allergies, and may have a viral infection. Many patients experience relief from allergic symptoms with antihistamines, decongestants, and nasal steroids. Reducing exposure to allergens can also be beneficial (for example, avoiding outdoor exposure during peak pollen times). To learn more about your allergies and effective treatments, schedule an in-person or telemedicine appointment with the allergy doctors at The Asthma Center.
Coronavirus (COVID-19): Symptoms and Reducing Risk
The current understanding of coronavirus infection is not complete, and the CDC is constantly updating their webpage with new recommendations. At this point, the virus is spread primarily from person to person. This can occur upon close contact (within 6 feet) or inhalation of mucous particles after someone infected with the virus sneezes or coughs. Coronavirus (COVID-19) can cause symptoms ranging from mild to severe. Symptoms include fever, cough, and shortness of breath. At this time, there is no vaccine or antiviral drug for treatment. People with COVID-19 should receive supportive care to relieve symptoms and protect vital organ function. Self-quarantine is also recommended to prevent spread of the virus to others.
CDC recommends the following to prevent spread of the virus and minimize risk:
• Avoid close contact with people who are sick
• Avoid touching your eyes, mouth, and nose
• Stay home if you are sick
• Wash your hands often with soap and water for at least 20 seconds, especially after bathroom use, before meals, and after nose blowing, coughing or sneezing. Use alcohol-based sanitizer if soap and water are unavailable.
• Disinfect household and workplace objects (cell phones, keyboards, door knobs, etc.) using regular cleaning spray or wipes • Cover your cough/sneeze with a tissue and then dispose of it in a closed container
• Follow CDC recommendations for facemask use:
o CDC does not recommend that healthy people wear a facemask to protect themselves from respiratory diseases, including COVID-19.
o Facemasks should be used by people with symptoms of COVID-19 to help prevent disease spread. Facemasks are also crucial for health workers and people who are providing care in close settings (at home or in a health care facility). This information on COVID-19 was adapted from the CDC website. For more information and updates, see the CDC webpage: https://www.cdc.gov/coronavirus/2019-ncov/index.html
Common Colds: Symptoms and Treatments
If you have a common cold, you may have a runny nose, with thin or thick and yellow mucous. You may also have a low-grade (less than 100 degrees) fever, sneezing, weakness and fatigue –symptoms you may be familiar with from having colds in the past. Symptoms may last 5-10 days. Treatment for the common cold may include decongestants, pain relievers, and cough suppressants. Since the common cold is a viral illness, antibiotics are not an effective treatment. Your Primary Care Physician should be consulted about effective treatment plans. Studies have shown that viral upper respiratory symptoms that last at least 7-10 days may be complicated by bacterial infections. In general, it is assumed that an acute bacterial sinus infection occurs if the upper respiratory symptoms have persisted beyond 10 days. Bacterial sinusitis is usually accompanied by thickened nasal drainage, nasal congestion, facial pressure (especially one-sided or focused in one particular sinus area), post nasal drip, decreased sense of smell, low-grade fever, cough, fatigue, dental pain and/or ear pressure. If bacterial sinusitis does not clear on its own, antibiotics may be prescribed.
It is important to note that antibiotics are not effective for the Common Cold or coronavirus. Overuse of antibiotics for viral illnesses can lead to development of antibiotic resistant “super germs”.
For further questions and to schedule an appointment, call The Asthma Center at 215-569-1111 (PA) or 856-316-0300 (NJ).
The information contained in this article is the sole property of The Asthma Center and may not be repurposed for other use without permission from The Asthma Center.
More Info
February 10, 2020. FDA Approves Peanut Allergy Treatment for Children!
Peanut allergy is a condition that can result in severe, life-threatening reactions. These allergic reactions occur in peanut-sensitive individuals when the body mistakes a peanut for a harmful invader. Recently, the FDA approved a new treatment called Palforzia (Peanut Allergen Powder) to reduce severity of reactions in the case of accidental exposure to peanuts. It is approved for children ages 4 – 17. The oral immunotherapy involves an initial dose, followed by a phase of up-dosing over a few months, and ultimately a maintenance phase. Because Palforzia contains peanut allergen, it is important that these doses be administered by a healthcare professional prepared to manage severe reactions, including anaphylaxis.
The Asthma Center will now offer oral peanut desensitization therapy, in addition to sensitivity evaluations for all foods. Although Palforzia does not cure peanut allergy, studies have shown that it effectively reduces risk of severe allergic reaction, and it may be an appropriate treatment for your child. Contact us to schedule an evaluation or learn more about this treatment option.
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
More Info
May 23, 2019. Memorial Day Allergy-Friendly Holiday Guide
Memorial Day Weekend is here! Read The Asthma Center’s board-certified allergists’ Memorial Day Allergy-Friendly Holiday Guide to keep the unofficial “start of summer” “sneeze-free.” Happy Memorial Day Holiday Weekend!
Memorial Day Allergy-Friendly Holiday Guide
This Memorial Day Allergy-Friendly Holiday guide from The Asthma Center Allergists is full of tips to help those with allergies, asthma, and sinus problems enjoy all the weekend celebrations and outdoor activities.
Memorial Day Allergy-Friendly Holiday Guide Tip #1: Reduce Pollen and Other Allergy Triggers
- Wear long sleeves and long pants when mowing the grass. Be sure to shower & wash your hair afterwards.
- Limit time outdoors during the early morning hours when the most pollen is released.
- Sleep with windows closed and drive with windows up.
- Wear wrap-around sunglasses or glasses outdoors to limit exposure of pollen to your eyes.
- Avoid wearing contact lenses, or switch to daily disposable contacts to avoid allergens building up on the lenses.
- Beware of tracking grass pollen into your home from overlooked sources that may “sneak” in on kids’ shoes and clothing, pets especially after playing outside in the grass, and on morning newspaper sleeves.
- Shower and wash your hair after extended outdoor exposure. Wash your hands and face frequently, including eyebrows.
- Change your pillowcase often.
Weather Conditions & Allergies
- Pollen and mold spore counts typically are highest during the morning hours.
- Pollen will be heaviest with hot, dry windy conditions.
- Thunderstorms, lightening & wind can all increase pollen in the air after a storm has passed.
- Mold spores thrive with heat and humidity.
Allergy- Friendly Grilling
Memorial Day weekend celebrations often mean “firing up the grill” for picnics and barbecues with family and friends. Did you know that red meat allergy can be triggered by bites from the Lone Star Tick, a variety of tick that is active and prevalent in our region? Learn all the facts in our recent blog Allergic to Red Meat? Lone Star Ticks to Blame.
Allergy – Friendly Gardening
Allergy sufferers who like to garden or are looking to buy flowers for the holiday weekend may experience dificulties around flowers and flowering plants. Fortunately, many flowers produce very little or no pollen. However, it is important to be mindful of the few that cause misery for allergic individuals. Avoid Pigweed, Chamomile, Chrysanthemums, Daisies, Goldenrod, & Sunflowers. For more information on flowers, plants, trees, and shrubs to avoid, check out our Tips for Allergy-Free Gardening & Indoor House Plants.
The “Priming Effect” & Allergies
Dr. Marc Goldstein explains, “The ‘priming effect’ is set up during the early periods of exposure to a pollen (as in the beginning of tree and grass pollen season). Depending on an individual’s level of allergic sensitivity, symptoms typically are experienced with higher levels of pollen. As the season progresses and exposure to the relevant pollen diminishes, “priming” accounts for why less pollen exposure in the air continues to provoke the same allergic misery.” Bottom line: This time of year, if you have allergies, symptoms may be triggered by even limited exposure to pollen and molds, and some individuals may also be more sensitivity to irritants such as pollutants, odors and smells that would not ordinarily cause symptoms.
The Asthma Center would like to take this time to wish all our friends, patients and staff a Happy Memorial Day! This weekend, we remember the men and women in our armed forces who died fighting for our country, and we thank them for their service.

Antihistamines Not Enough Allergy Relief?
If reducing your exposure to pollen in combination with over-the-counter antihistamines and nasal sprays don’t work on your symptoms, it’s still not too late to get relief. A board-certified Allergist can help.
At The Asthma Center, our allergists and pediatric allergists help our patients manage their allergies by determining what local spring allergens cause symptoms. For example, with spring allergies, we identify which local trees (including Oak, Pine, Mulberry and Birch) and grasses (including June, Kentucky Blue, Meadow Fescue, Orchard, Perennial Rye, Redtop, Sweet Vernal and Timothy) trigger allergy symptoms by using minimally invasive in-house diagnostics, like allergy skin testing. Pairing these results with local knowledge of allergy triggers like pollen, ragweed and mold, our allergists develop personalized plans that treat not only the symptoms but also the cause of allergies. And because allergy symptoms often spike with pollen, we know exactly when to adjust allergy medication – providing more relief when conditions are bad and less medication every time else.
The National Allergy Bureau is a nonprofit organization affiliated with the American Academy of Allergy, Asthma, and Immunology that oversees and certifies pollen counting stations across the US. The Asthma Center operates the only certified pollen and mold stations in the Delaware Valley, with one location in Philadelphia and the other in South Jersey (Mount Laurel, NJ). You can follow our local pollen counts on our website, Facebook page, and direct to your inbox by subscribing for free here.
The Asthma Center is the Delaware Valley’s Official Pollen and Mold Spore Count Station

Our allergists, pediatric allergists, and asthma specialists treat patients in 9 convenient locations throughout the Delaware Valley.
PA: (215) 569-1111 ![]() NJ: (856) 235-8282
NJ: (856) 235-8282
Center City Philadelphia • Society Hill Philadelphia • Northeast Philadelphia
The Main Line – Bala Cynwyd PA
Mt. Laurel NJ • Woodbury NJ • Hamilton – Princeton NJ • Forked River NJ
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
For interviews and tours of the Delaware Valley’s only certified pollen and mold spore stations for the National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com.
If interested in purchasing historical pollen and mold spore counts, please email gwoodlyn@asthmacenter.com for information.
More Info
March 18, 2019. 2019 Tree Pollen (Spring Allergies) in Philadelphia and South Jersey Starts Now
Daily Delaware Valley Official Pollen, Ragweed, and Mold Spore Counts Resume
2019 Tree Pollen (Spring Allergies) in Philadelphia and South Jersey Starts Now
Tree Pollen – Are you feeling those old familiar, or new and different, symptoms of itchy watery eyes, and sneezing? Nearly everyone is ready for sunny skies and warm days, but springtime also brings spring allergies (Top Spring Allergy Signs and Symptoms). In the Delaware Valley last week, with temperatures climbing to nearly 70 degrees on several days, The Asthma Center began monitoring “what’s in the air?,” and we are please to announce the return of official daily Pollen and Mold Spore Counts.
You can follow our local pollen counts on our website, Facebook page, and direct to your inbox by subscribing for free here.
Why Am I Sneezing Now? Why Are My Eyes Watering?
Typically, juniper/cedar trees are the “early bloomers” in the metropolitan Philadelphia-South Jersey area, along with maple and elm tree pollen, and The Asthma Center’s first air sample late last week confirmed the presence of tree pollen. Over the past 10 years, the onset of spring pollen was observed at the beginning the second week of March. However, last year (the 2018 season) later than usual, but also began with heavier concentrations of pollen at the onset of the spring season compared to previous years observed by The Asthma Center. Now, the onset of the 2019 spring pollen season appears similar to 2018’s spring season start.
This week’s “cold snap” is expected to be brief. Prolonged periods of less than 40 degrees may close up the buds on trees temporarily (the ones that burst open last Thursday and Friday with highs nearly reaching 80 degrees.) Weather forecasts for the next ten days predict mostly dry and increasingly warmer weather. As temperatures quickly rebound, expect heavy tree pollen, grass pollen joining in, and the full onslaught of spring allergies.
What Is Pollen and How Do We Count It?
Trees and other plants reproduce by creating pollen grains, a fine “dust,” that is often visible to the naked eye (all that yellow or green dust on cars in the morning), but other times so small that it can only be seen under a microscope. Not all pollen cause allergy symptoms, but those that do are light and can travel far on wind currents.
Trees pollinate for two to three week intervals at various times and overlap with peaks observed in our region from late April through early May. Similar to tree pollen, grass pollen is produced as a means of reproduction and depends on wind currents to be transported. Airborne grass pollen appears in early April, peaks throughout May, and declines in June. The Delaware Valley also experiences a second burst of grass pollen in September. Weed pollen are prevalent later in the summer, with ragweed pollen a major culprit in our area.

Throughout spring pollen season, we operate two monitoring stations: one on a rooftop in Center City Philadelphia and the other in Mount Laurel, NJ. The Asthma Center publishes these daily pollen, mold, and ragweed counts through the spring, summer and fall and provides a free daily (Monday – Friday) pollen and mold count subscription service. (Subscribe for free here.)
What Are Pollen Allergies?
In the presence of allergy triggers like tree pollen, the body reacts by creating histamine among other chemicals. This reaction causes the allergy symptoms we typically feel in spring like sneezing, itchy and watery eyes, and congestion. While symptoms are often similar, people react to different allergy triggers – some people are allergic to the juniper that’s in the air today, but others not. It just depends! Many allergy sufferers use the daily counts to keep track and prepare for their symptoms by starting allergy medication.
Pollen allergy treatment options often include antihistamines, nasal steroid sprays, decongestants, and mucus thinners. Off the shelf products can be extremely effective for treating symptoms, but because everyone’s allergies are unique, they may not work well for everyone. Another powerful option is allergy immunotherapy (allergy shots). Based on the results of the allergy skin tests which determine a person’s specific allergy triggers, allergy shots are custom formulated for each individual to treat their specific allergies. People typically experience significant, long term improvement using this methodology.
Delaware Valley’s Only Official Pollen and Mold Spore Counts (NAB Certified)
The National Allergy Bureau is a nonprofit organization affiliated with the American Academy of Allergy, Asthma, and Immunology that oversees and certifies pollen counting stations across the US. The Asthma Center operates the only certified pollen and mold stations in the Delaware Valley, with one location in Philadelphia and the other in South Jersey (Mount Laurel, NJ).

Call A Location Near You – Ask About Our Spring Saturday Hours
Center City Philadelphia • Society Hill Philadelphia • Northeast Philadelphia
Mt. Laurel NJ • Woodbury NJ • Hamilton – Princeton NJ • Forked River NJ
For interviews and tours of the Delaware Valley’s only certified pollen and mold spore stations for the National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com.
If interested in purchasing historical pollen and mold spore counts, please email gwoodlyn@asthmacenter.com for pricing information.
The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
More Info
March 1, 2019. Spring Allergy Season Coming Soon to Philadelphia and South Jersey
Spring Allergy Season Coming Soon to Philadelphia and South Jersey
Though it still may feel like winter, trees in the Philadelphia and South Jersey area are focused on spring, which means spring allergy season is soon to come.
According to Dr. Donald Dvorin, a board certified Allergist, from The Asthma Center and Delaware Valley’s official pollen and mold spore counter, cold days and nights are preventing most tree buds from opening and thus holding off the release of pollen. Over the past 10 years, spring pollen has generally been present at the beginning of the second week of March. However, the spring seasons for 2018 and 2017 had unusual beginnings, and may hold clues for what we can expect with the upcoming spring 2019 pollen season.
The Asthma Center Outlook – When Will Spring Allergy Season Begin?
First of all, in 2017, warm spring-like temperatures arrived early (74 degrees on 3/1/2017 and 62 degrees on 3/2/2017) which contributed to Dr. Dvorin observing extreme levels of tree pollen during the first week of March. In contrast, winter weather clung to our region in 2018 including a late Nor’easter that brought snow the third week of March and delayed onset of the spring allergy season for several weeks.
Based on historical data from National Weather Service, it appears that the 2019 weather for our region is following patterns similar to 2018 (see below). According to the “Monthly Forecast” from Accuweather and the “Long Range Outlook” from EPAWA Weather Consulting, the Delaware Valley can expect March to bring a variety of weather conditions.
Spring 2019 Tree Pollination Onset
First Week (March 4rd – March 10th): Low/Weak outlook for “early” onset of spring tree pollination.
- Winter holds on with cold temperatures (Highs predicted between 28 – 40 degrees and Lows consistently below freezing, possibly dropping into the teens on some nights. Chances for snow are considered high.
Second Week (March 11th – March 17th): Possible but Unlikely outlook for “typical” onset of spring tree pollination.
- Spring-like temperatures and pleasant days are likely. Nights will still be chilly with lows barely above freezing.
Third Week (March 18th – March 24th): High/Strong outlook for “delayed but heavy” onset of spring tree pollination.
- Chances for rain are considered moderate, but Highs are predicted to consistently range between in the mid-50s. Overnight lows are expected to stay above freezing.
Finally, as the weather warms, we will see a surge in pollen as trees across the region start to bloom. Locations further south (e.g. Alabama, Florida, Carolinas) have already reported high levels of tree pollen.
|
Average Temperature |
2019 |
2018 |
2017 |
|
January |
33.3 |
32.8 |
38.5 |
|
February |
37.3 |
41.9 |
44.2 |
|
March |
|
40.1 |
42.1 |
|
Average Precipitation, Snow & Ice |
2019 |
2018 |
2017 |
|
January |
6.5 |
7.5 |
8.6 |
|
February |
9.9 |
7.4 |
3.3 |
|
March |
|
19.9 |
11.3 |
Local Daily Pollen Counts
Dr. Donald Dvorin has monitored and analyzed our region’s pollen with a Burkard Spore Trap Device, which samples the air by trapping pollen and other airborne molecules on a greased slide. Every morning, he removes the slide and examines it under a microscope. Different plant pollen have unique shapes, so he can count how much of each plant pollen is on the slide and use that metric to determine the daily pollen count. The Asthma Center publishes these daily pollen, mold, and ragweed counts through the spring, summer and fall and provides a free daily (Monday – Friday) pollen and mold count subscription service. ( Subscribe for free here. ) The Asthma Center expects pollen counts to resume mid March.

Delaware Valley’s Only Certified Pollen/Mold Counting Station
The National Allergy Bureau is a nonprofit organization affiliated with the American Academy of Allergy, Asthma, and Immunology that oversees and certifies pollen/pollen counting stations across the US. The Asthma Center operates the only certified pollen/mold stations in the Delaware Valley, with one location in Philadelphia and the other in South Jersey-Mount Laurel, NJ.

You can follow our local pollen counts on our website, Facebook page, and direct to your inbox by subscribing for free here.
The Asthma Center is the Delaware Valley’s Official Pollen Count Station.
PA: (215) 569-1111 ![]() NJ: (856) 235-8282
NJ: (856) 235-8282
Center City Philadelphia • Society Hill Philadelphia • Northeast Philadelphia
Mt. Laurel NJ • Woodbury NJ • Hamilton – Princeton NJ • Forked River NJ
For interviews and tours of the Delaware Valley’s only certified pollen and mold spore stations for the National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com.
If interested in purchasing historical pollen and mold spore counts, please email gwoodlyn@asthmacenter.com for pricing information.
More Info
October 4, 2018. Flu Shot – How to Pick The Right One?
Get the Flu Shot That’s Right for You!
The Asthma Center physicians and staff get flu shots too! In the above picture taken in The Asthma Center’s Woodbury, NJ office, Clinical Supervisor Sandy Richards, RN administers the quadrivalent flu shot to Medical Secretary Michelle Wood! (Courtesy: staffer Shannon Cephas, LPN)
Flu Season 2018 – 2019 is Here
According to the Centers for Disease Control and Prevention (CDC), flu shots are recommended for everyone 6 months and older. The flu vaccine is one of the most important steps you can take to prevent getting the flu.
Last year was a particularly devastating year from influenza infections. According to the CDC, 80,000 Americans died of flu and related complications – the highest death toll associated with the flu in over 40 years. Over 90% of deaths were in adults >65 years while 180 children/teens died from influenza and related complications. It is difficult to predict whether this year’s flu will be as aggressive. The best way to protect yourself and your children is to get properly vaccinated. With several different flu vaccines available, here’s a guide to which option is best for you.

Flu Shot FAQ: Not All Flu Shots are Created Equal
- Four is Better Than Three (for everyone under age 65)
The Asthma Center highly recommends the quadrivalent (4 strain) influenza vaccine for all patients under the age of 65 years. The quadrivalent vaccine contains the four most common types of the influenza virus versus only three types in the older trivalent (3 strain) vaccine and provides the most complete protection for this age group against the flu this winter.
- Three with Extra Power (for everyone age 65 and older)
The Asthma Center highly recommends the high potency trivalent (3 strain – high potency) influenza vaccine for all patients 65 years and older . This is the vaccine administered by our practice because it provides the most complete flu protection for this age group. Note that this is superior to the standard trivalent vaccine.
- Buyer Beware – Not All Flu Shots Are The Same
Many local pharmacies and other medical facilities have continued to administer the least protective trivalent influenza vaccine when a patient asks for a “flu shot”. Be sure to ask for the quadrivalent formulation or the high potency trivalent, depending on your age.
- What Parents Need to Know
Children are a particularly vulnerable group when it comes to the flu. The Centers for Disease Control and Prevention (CDC) recommends that everyone 6 months and older get the flu shot every flu season.

- What about Nasal Spray Flu Vaccines?
This year, the CDC is recommending the FDA approved nasal spray vaccine (FluMist, which is a live attenuated quadrivalent vaccine) in age appropriate individuals who do not have asthma!
- Can you get the Flu Shot if you are egg-allergic?
With a history egg-allergy of any severity, the CDC does still recommend that any of the age appropriate flu vaccines that are available. Special challenges or two-step same day inoculation may be required in some cases.
- Can You Have a Reaction to the Flu Shot?
Unlikely, but yes.
At The Asthma Center, our board-certified allergists and highly trained staff are well equipped to handle adverse reactions. All of our physicians and staff are trained to recognize and treat reactions to any vaccine, including the flu shot.
- Experience & Customized Care
At The Asthma Center, we personalize your experience by choosing the form of the influenza vaccine that is right for you – multiple doses for young children (if necessary), preservative-free for those with preservative sensitivities, high-dose for those over 65 years of age and the quadrivalent vaccine for those not requiring alternative formulations. And, most importantly, we are there for you in the unlikely event you experience an adverse reaction to the vaccine.
Did you know that you should wait for 30 minutes after administration of any vaccine so that if an immediate severe reaction (anaphylaxis) occurs, you can be immediately treated?
Center City Philadelphia • Society Hill Philadelphia • Northeast Philadelphia
Mt. Laurel NJ • Woodbury NJ • Hamilton – Princeton NJ • Forked River NJ
For questions regarding flu shots, please email Gaille at gwoodlyn@asthmacenter.com. The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease.
More Info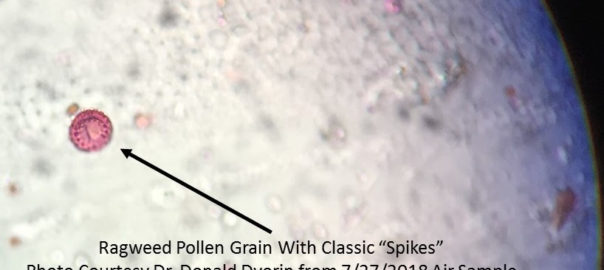
July 31, 2018. Record Early Ragweed Season In Philadelphia
Philadelphia, PA – July 27, 2018 – Record early ragweed season in Philadelphia, as recorded by the ragweed pollen counting station at The Asthma Center.
Record Early Ragweed Season Start in Philadelphia
What’s Normal for Ragweed Season?
What About Ragweed Pollen This Year?
What to Do About Ragweed Allergies?
With ragweed season coming early and promising to be extremely strong, here are a few tips for treating ragweed allergy symptoms from our allergists:
1. Start allergy & asthma medications before your symptoms start. This is one of the most important measures you can take to minimize seasonal allergy symptoms.
2. Know your level of pollen sensitivity and monitor pollen levels. To find out if you are allergic to ragweed, Allergy Skin Testing is one of the most reliable methods to determine allergy sensitivity, particularly when correlated with your personal history. Free subscribers of The Asthma Center’s daily email receive pollen, mold, and ragweed counts direct to their inbox.
3. Keep pollen and mold spores out of your nose, eyes, ears, lungs and home.
Philly’s Only Certified Ragweed Pollen Counts
The Asthma Center operates the only certified pollen and mold stations in the Delaware Valley, with one location in Philadelphia and the other in South Jersey (Mount Laurel, NJ). The National Allergy Bureau is a nonprofit organization affiliated with the American Academy of Allergy, Asthma, and Immunology that oversees and certifies pollen counting stations across the US. You can follow our local pollen counts on our website, Facebook page, and direct to your inbox by subscribing for free here.
The Asthma Center is the Delaware Valley’s Official Pollen and Mold Spore Count Station

PA: (215) 569-1111 ![]() NJ: (856) 235-8282
NJ: (856) 235-8282
Center City Philadelphia • Society Hill Philadelphia • Northeast Philadelphia
The Main Line – Bala Cynwyd PA
Mt. Laurel NJ • Woodbury NJ • Hamilton – Princeton NJ • Forked River NJ
For interviews and tours of the Delaware Valley’s only certified pollen and mold spore stations for the National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com. The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease. If interested in purchasing historical pollen and mold spore counts, please email gwoodlyn@asthmacenter.com for information.
More Info
May 11, 2018. Simple tips for an allergy-friendly Mother’s Day full of flowers and celebration.
Philadelphia, PA – May 10, 2018 – Mother’s Day is here! As flowers are symbols for both Mother’s Day and allergies, The Asthma Center’s board-certified allergists are happy to share our guide to enjoying Mother’s Day flowers with allergies to keep your celebration “sneeze-free.” Happy Mother’s Day!
Mother’s Day Flowers & Bouquets: An Allergy-Friendly Guide
Individuals with respiratory allergies may experience symptoms around flowers and other plants when indoors or in outdoor gardens. Fortunately, there are many flowers, shrubs, trees, and grasses that produce very little or no pollen and can be used in indoor and/or outdoor environments to reduce allergy symptoms.
The pollen from flowers used in arrangements is heavier than tree, grass and weed pollen. This means that usually it is less of a trigger for allergy and asthma symptoms, but it may still cause problems. Here’s our allergists’ favorite tips to keep in mind when giving or receiving flowers as a gift:

- Before you bring any ornamental flowers indoors, remove the stamen to reduce as much pollen as possible.
- Wipe stems, leaves, and petals as needed to remove pollen.
- Resist the temptation of placing your nose directly in a bouquet of flowers or touching the flowers – direct contact on the hands, other parts of the skin, eyes or nose may trigger allergy symptoms.
- The fragrance from some plants may also have a very significant irritant effect if you have respiratory allergies and/or asthma. Try to avoid particularly fragrant flowers.
- Reduce symptoms by avoiding the “worst offenders” such as chamomile, chrysanthemums, daisies, goldenrod, and sunflowers. Choose allergy-friendly flowers instead:
Mother’s Day Flowers: Allergy Friendly
For those with allergies, the best way to include flowers with Mother’s Day is to choose allergy-friendly flowers. These flowers produce less pollen and fragrance, so result in less symptoms:
- Begonia
- Clematis
- Columbine
- Crocus
- Daffodil
- Geranium
- Hydrangea
- Iris
- Lily
- Periwinkle
- Rose
- Tulip
- Zinnia
Fun Fact: Only male plant species produce the pollen that people react to, so that if you are able to purchase flowers from female plants you can be sure that they do not produce pollen.
Check out Dr. Marc Goldstein discussing allergy-friendly flowers and bouquets.
Philly’s Only Certified Pollen Source
The National Allergy Bureau is a nonprofit organization affiliated with the American Academy of Allergy, Asthma, and Immunology that oversees and certifies pollen counting stations across the US. The Asthma Center operates the only certified pollen and mold stations in the Delaware Valley, with one location in Philadelphia and the other in South Jersey (Mount Laurel, NJ). You can follow our local pollen counts on our website, Facebook page, and direct to your inbox by subscribing for free here.
The Asthma Center is the Delaware Valley’s Official Pollen and Mold Spore Count Station

Ask about our Special Spring Saturday Hours for New Patients (available in selected locations)!
PA: (215) 569-1111 ![]() NJ: (856) 235-8282
NJ: (856) 235-8282
Center City Philadelphia • Society Hill Philadelphia • Northeast Philadelphia
The Main Line – Bala Cynwyd PA
Mt. Laurel NJ • Woodbury NJ • Hamilton – Princeton NJ • Forked River NJ
For interviews and tours of the Delaware Valley’s only certified pollen and mold spore stations for the National Allergy Bureau (NAB) certified pollen, ragweed, and mold spore counting stations in Philadelphia, PA and Mt. Laurel, NJ, please email gwoodlyn@asthmacenter.com. The health information contained in this article is meant for basic informational purposes only. It is not intended to serve as medical advice, substitute for a doctor’s appointment or to be used for diagnosing or treating a disease. If interested in purchasing historical pollen and mold spore counts, please email gwoodlyn@asthmacenter.com for information.
More Info