Uncategorized

February 19, 2024.
Xolair: First FDA Approved Drug for Food Allergies
What is Xolair?
On Friday, February 16, 2024, the FDA approved the first ever drug, Xolair (omalizumab), for the treatment of food allergies for children one year and older, and for adults. This is a revolutionary approach for the treatment of food allergies and can now be prescribed by the food allergy doctors at The Asthma Center.
The approval of Xolair was based on a multicenter US study involving 168 adults and children greater than 1 year old, allergic to peanuts and at least 1 other food. Xolair treated individuals had a statistically significant reduction of food allergic reactions upon food challenges in comparison to placebo treated individuals.
What are common food allergies?
Millions of Americans (about 6 percent of the US population) have food allergies putting them at risk for potentially life-threatening allergic reactions called anaphylaxis. It is estimated from the USDA (2023) that food anaphylaxis results in 30,000 emergency room visits, 2,000 hospitalizations, and 150 deaths in the US per year.
The nine most common causes of food allergies in the US include: milk, egg, fish, Crustacean shellfish (crab, shrimp, lobster), tree nuts (e.g. almonds, walnuts, cashews, pecans), peanuts, wheat, soybean, and sesame.
What does Xolair treat?
Xolair is a monoclonal antibody biologic drug that was originally approved in 2003 for treatment of moderate to severe asthma and subsequently approved for chronic hives and chronic rhinosinusitis with nasal polyps. In February 2024, Xolair was approved to help treat food allergies.
Can Xolair be used to treat food allergies?
Yes, Xolair can be used to treat food allergies. It was approved in 2024 to help reduce allergic reactions to food(s) after accidental exposure, however it is not approved for immediate emergency treatment of allergic food reactions like food-induced anaphylaxis. Individuals with food allergies, even on Xolair, will need to continue adhering to strict food avoidance.
Can Xolair be used to treat food allergies in kids? Can Xolair be used to treat food allergies in adults?
Yes, Xolair can be used to treat food allergies in kids one year old and older, as well as in adults.
How is Xolair used for food allergy treatment?
Xolair is administered by injection by a medical professional in a medical office. For food allergy treatment, it is injected every 2 to 4 weeks.
This treatment reduces the risk of severe food allergic reactions (anaphylaxis) that occurs with accidental exposure to one or more foods. Xolair is not approved for the emergency treatment of food allergic reactions and therefore strict food avoidance should still be continued.
Does The Asthma Center Treat Food Allergies with Xolair?
Yes, the food allergy doctors at The Asthma Center use Xolair to treat food allergies. Patients are first evaluated by our allergy doctors for their history of food-induced allergic reactions. Our doctors then can test for food allergies using skin test(s) and/or blood test(s). After diagnosing the complete range of food allergies, our allergy doctors will discuss with you the option of using Xolair for the treat of food allergies. To learn more about this revolutionary new treatment option for food allergies, please see Xolair for Food Allergy Treatment.
Our food allergy doctors treat patients for food allergies in the Philadelphia area and South Jersey at our locations:
Center City Philadelphia • Northeast Philadelphia
More Info
December 12, 2022. TRIPLENDEMIC: RSV, COVID-19 or Flu
We are currently experiencing concurrent emerging cases of RSV, COVID-19, and influenza virus causing acute respiratory symptoms in children and adults.. Flu cases started earlier than usual this season and there is an increased number of cases of respiratory syncytial virus infection commonly known as RSV with new COVID-19 Omicron subvariants. COVID-19 in the meantime is starting to increase with increasing trends of admissions and hospitalizations throughout most parts of the country. These viruses will continue to spread as we head into the winter. Fortunately, for the past two years, RSV and flu have been less problematic as people had observed masking and social distancing decreasing the rate of transmission. Therefore, lack of exposure over the past two years has left most people, particularly children, with lower levels of protection and more vulnerable to the current respiratory virus season. In addition, there has been a relaxation of COVID-19 precautions, so transmission of respiratory viruses will continue to increase for all three viruses as we head through the winter months.
How do I know if I have RSV vs COVID vs Flu?
The symptoms of RSV, COVID, and influenza can be very similar, making it difficult to make a clinical distinction between the three. With RSV, COVID, and flu, people can experience cough, sore throat, fever, and runny nose. You can test for COVID at home with COVID antigen tests whereas testing for influenza and RSV must be done in a health facility. Home assays for FLU & RSV have not been developed yet.
What are the health risks of COVID vs Flu vs RSV?
Those who are at greater risk of having serious disease from RSV, COVID, and flu (influenza) includes the very young and very old as well as those who have certain underlying health conditions. Symptoms can progress quickly and spread throughout the household making it difficult for work and school attendance and following normal routines. Even mild infection with COVID can lead to longer term symptoms called long COVID that can produce issues with brain fog, extreme fatigue and palpitations of the heart.
Are there vaccines for COVID vs Flu vs RSV?
There is not yet a single vaccine for COVID, flu and RSV. There is a standalone COVID vaccine and a standalone flu vaccine. There is no vaccine for RSV.
For COVID, there is an updated bivalent COVID vaccine that recently became available for those who are 5 and older and who have already gone through primary COVID monovalent vaccinations. For the flu vaccine, this year, there seems to be a good match between what we are seeing currently in terms of the dominant influenza strain H3N2 and what is covered in this year’s influenza vaccine, which means that the flu vaccine will be effective in helping reduce the severity of flu symptoms.
There are several forms of the influenza vaccination that can be obtained depending on your age, previous reactions to preservatives, and preference for route of administration. It usually takes two to three weeks to develop an immune response to the vaccine, so it is recommended that people get vaccinated if they have not received their influenza vaccination at this time. Influenza cannot only cause acute respiratory symptoms in the nose and the chest, but can lead to more severe infection and in some cases death. At this time, it is difficult to determine whether the influenza season will result in more severe cases resulting in hospitalization and death, however, vaccine protection would help decrease the chance of severe outcome.
What is RSV? Is there a RSV vaccine?
RSV infections are due to a virus that infects the respiratory tract and typically causes a mild cold like syndrome in most older children and adults, but can be very dangerous and deadly in very young children, particularly babies under 1 and in the elderly. An RSV vaccine is currently not available, but is being developed in the United States. The only way to establish immunity to RSV is really through an infection. Since the COVID pandemic, RSV cases dropped off makes young children less likely to have developed immunity from past infection. The virus typically will circulate this time of the year throughout the winter and young children who have not been exposed are being hit now and causing dramatic increase in hospitalizations in pediatric hospitals.
What can you do to decrease your chance of getting sick from RSV, COVID, and flu (influenza)?
To reduce your chances of getting sick from RSV, COVID, or the flu, it is important to get fully vaccinated to the flu (influenza) as well as COVID-19, particularly the bivalent booster that is currently available that protects against the currently circulating Omicron variants. In addition, to prevent transmission of all viral illnesses, hand washing, coughing or sneezing into your elbow is important to prevent transmission, wearing a mask is appropriate in public settings and staying home if you are symptomatic to recover quickly and prevent transmission rates. Improved ventilation in indoor environments also will help decrease transmission rates. In cases where symptoms seem to be progressing particularly in young children and adults, antiviral therapy or monoclonal antibody therapy may still be appropriate for patients who have acute COVID to prevent progression to severe infection or development of long-term COVID symptoms. Supportive therapy for any other respiratory complications may also be required in cases of influenza, COVID or RSV. Antiviral therapy for influenza may also be appropriate with the acute onset of symptoms and/or for those who are exposed to individuals with documented acute influenza.
More Info
November 10, 2021. South Philly Fire Presents Problems for Those with Asthma and COPD
Yesterday afternoon the news of a large 2 alarm fire in Southwest Philadelphia hit headlines across the region. While it is still not clear exactly what started the blaze, officials say that it stemmed from several small debris fires at a junkyard. As seen in the photo above, winds have carried smoke and fumes all the way to Southern New Jersey.
Due to the contents and size of this fire, it is very important for those in the Philadelphia and New Jersey area with heart and lung problems to minimize outdoor exposure until the air quality improves. This is an instance when wearing a mask when outside is especially important, whether around other people or not. Not only are masks effective protection against the spread of COVID-19, they also filter out harmful materials caused by fire. Acute particulates found in smoke can affect symptoms in patients with conditions such as Asthma and COPD. As shown in the graphs from Purple Air below, the fire caused a spike in particulates in the air from Philadelphia to Camden.
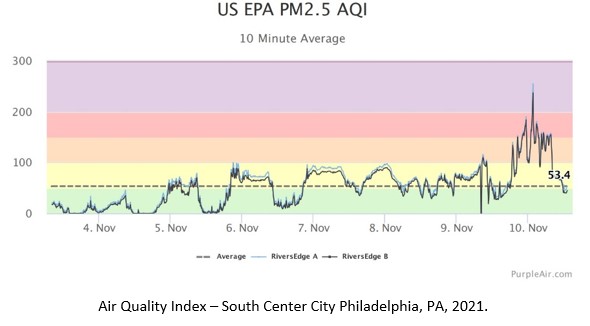
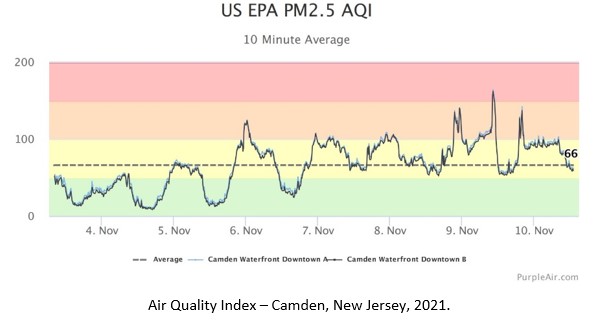
Certainly, maintain medications as directed, use rescue inhalers as needed, and feel free to contact The Asthma Center with questions or concerns.
More Info
January 19, 2021. Understanding Seafood Allergies
Prevalence of Seafood Allergies & Sub-group Allergies
Allergies to seafood are the most commonly reported allergy for adults and are among the most common for young children. Seafood allergies affect about 1-3% of the general population, with allergy to shellfish specifically being the most common and tending to cause more severe reactions and emergency department visits. Seafood allergy can be split into two categories: fish allergy and shellfish allergy. Fish (vertebrates with bony spines) allergy can include allergies to species like the following: salmon, tuna, and cod. Shellfish (invertebrates with no bony spine) allergy is further broken down into crustacean allergy (shrimp, lobster, crab, etc.) and mollusk allergy (snails, mussels, clams, oysters, etc.). Many individuals who are allergic to one type of shellfish are also allergic to the other. Crustacean allergy is more common than mollusk allergy. Geographic distribution and varying dietary patterns also influence the prevalence of shellfish allergies; for example, shellfish allergy is considered more common in Asian countries, where shellfish is more often consumed, than in, for instance, the US.
Shellfish allergy throughout life
Shellfish allergy can develop at any age throughout life and can be persistent, even for those with new onset shellfish allergy. Some individuals, on the other hand, can experience an allergic reaction the first time they eat shellfish.
Causes of seafood allergy
Fish allergies are primarily caused by parvalbumins, a type of calcium-binding protein. Other allergens that can cause fish allergy include enolases and aldolases, two enzymes, and fish gelatin. The major allergens in shellfish allergy are muscle proteins called tropomyosins. Other allergens in shellfish allergy include myosin light chain (a muscle protein), arginine kinase (an enzyme), and hemocyanin (a protein in mollusks that carries oxygen).
Mechanism of seafood allergy
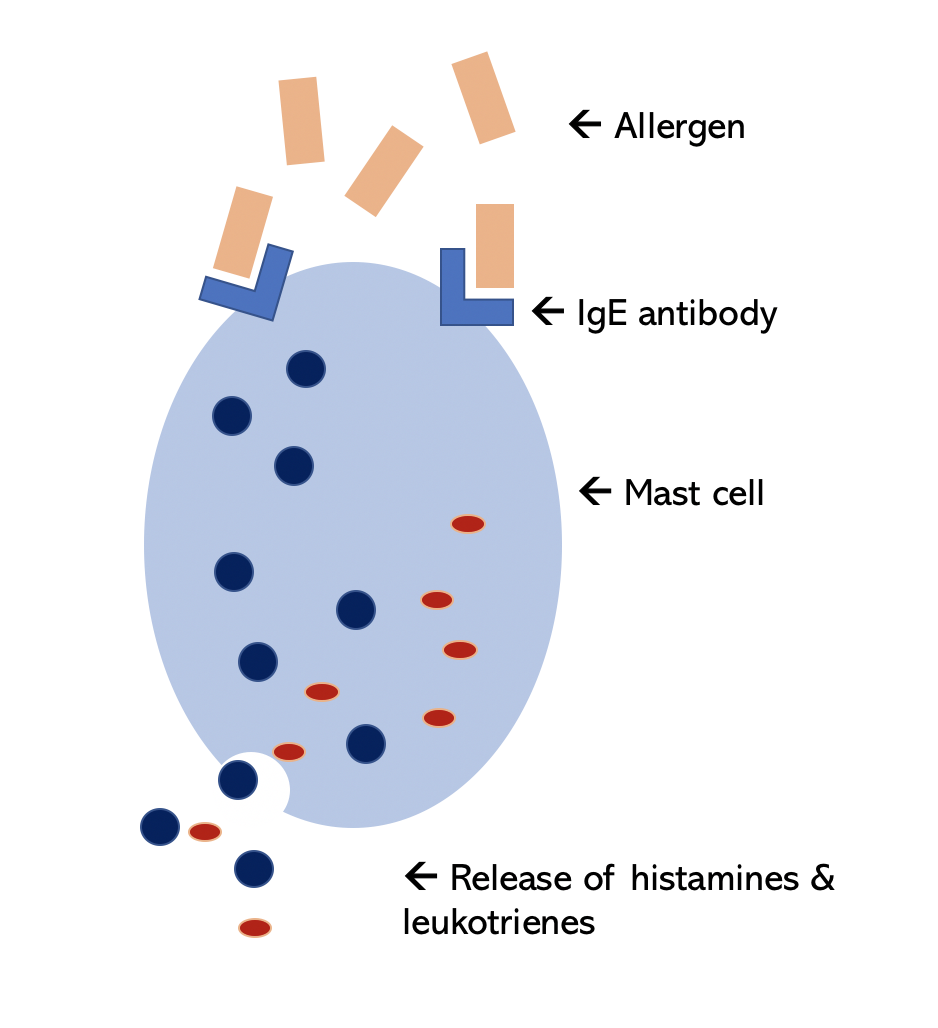
Most allergic reactions occur in response to recognition to the above allergens by allergy antibodies known as IgE antibodies. After exposure, the body produces antigen-specific (for example tropomyosin-specific) allergy IgE antibodies. These specific IgE antibodies bind to mast cells (a specific type of immune cell), and can also bind to allergens (like tropomyosin) when exposed. Binding the allergen to the specific IgEs on mast cells spurs an allergic immune response, prompting mast cells to release histamine and other inflammatory chemicals to produce allergy symptoms.
Symptoms of seafood allergy
These reactions often present within one hour of ingestion. Common symptoms include:
- Hives (urticaria)
- Shortness of breath (dyspnea)
- Throat tightness
- Deep swelling of various body parts (angioedema)
- Respiratory symptoms
- Swelling of vocal cords and epiglottis that can cause airway obstruction (laryngeal edema)
- Severe allergic reaction (anaphylaxis) involving multiple body parts and often occur with a drop in blood pressure
Contact dermatitis
Contact dermatitis is another allergic reaction that can occur after handling seafood. Contact dermatitis is characterized by an allergic skin reaction, usually red, itchy, and swelling in the general spot of contact. This reaction occurs in response to the allergic proteins that enter the skin after contact and often occurs after previous sensitization. Contact allergies to shellfish may occur in the absence of respiratory or GI symptoms. These reactions can take anywhere from minutes to hours to occur.
Inhalation of allergens
Inhalation of seafood allergens, for example during cooking or processing, can also cause allergic reactions to the inhaled proteins. These reactions can cause symptoms similar to asthma.
Cross-reactivity
Cross-reactive allergens are similar proteins present in different substances. The proteins share the majority of amino acid sequences, the building blocks of protein, stimulating production of allergy antibodies (IgEs) that can react to similar appearing proteins across different substances. Cross-reactivity is high (91-100%) amongst shellfish species as well as some non-shellfish substances due to the presence of shared cross-reacting tropomyosin and other muscle protein allergens. Therefore allergic reactions to crustaceans and mollusks may be due to cross-reacting proteins found in crickets, cockroaches and dust mites.
For example, shellfish and house dust mites have similar tropomyosin structures (sharing around 80% similarity). Thus, it is suspected that frequent exposure through inhalation of non-shellfish sources, like house dust mites, may sensitize the individual to cause shellfish allergy by stimulating production of IgE to tropomyosin and other muscle proteins, then causing reactions to shellfish upon ingestion. For each person with diagnosed seafood allergy, it is imperative to also consider and test for cross-reactive proteins in dust mites and cockroaches.
Seafood allergy and iodine allergy
A common misconception is that individuals with shellfish allergy cannot take iodine or radio contrast material (RCM), which is used for contrast radiologic studies like CT scans and angiograms. This is not true. Previously it was believed that the iodine caused allergic reactions, but now it is known iodine itself does not cause allergies or shellfish allergy. Thus, patients with shellfish allergy are not at greater risk of reacting to RCM than non-shellfish allergic patients. Individuals with shellfish allergy are not at greater risk of reacting to iodine and individuals who react to iodine-containing products (like Betadine or povidone) are not at greater risk of reacting to shellfish.
Seafood-dependent exercise-induced anaphylaxis
Exercise-induced anaphylaxis can be triggered by ingestion of certain foods followed by exercise or exertion. Shellfish is a common cause of food-dependent exercise-induced anaphylaxis. Symptoms are usually similar to those of anaphylaxis (flushing, hives, fatigue, swelling of the face or extremities, gastrointestinal symptoms, and hypotension) and can begin during or after exercise. Usually, stopping exercise and avoiding food before exercise helps remedy this.
Pseudo-allergy or masqueraders of shellfish allergy
Anisakis reactions
An allergic reaction to a parasite called Anisakis simplex is another form of pseudo-seafood allergic reactions, that often go underreported and underdiagnosed. Anisakis is a small worm commonly found in seafood that infects these sea creatures through ingestion. These worms can affect humans if the Anisakis-ingested seafood is eaten without being fully cooked. This parasitic worm can be present in salmon, herring, cod, mackerel, squid, halibut, red snapper and shellfish, like shrimp. The allergic reactions produced are due to allergy IgE antibodies directed against Anisakis rather than to the seafood itself.
Anisakis reactions have been shown to cause symptoms ranging from acute or chronic hives (urticaria) to anaphylaxis. Understanding this allergy is important because Anisakis allergy may masquerade as a seafood allergy. Blood testing can be used to identify IgE antibodies specific to the Anisakis allergens.
Food protein-induced enterocolitis syndrome (FPIES) in children and adults
Enterocolitis is an inflammation of the small intestine and colon, both of which are parts of the digestive system. Symptoms can appear hours after ingestion and can include vomiting and diarrhea. In some cases this reaction can worsen to dehydration and low blood pressure. This is not an IgE-mediated reaction but instead is thought to be in response to other immune cells called T-lymphocytes and their inflammatory proteins (called cytokines). FPIES is presented in early infancy but usually resolves in childhood. Adults can experience an enterocolitis-like reaction as well, often after repeated exposure to a suspected food.
Scombroid poisoning
Scombroid poisoning, also known as histamine poisoning, is another seafood-related reaction that is often confused with seafood allergies. Scombroid poisoning typically results from eating spoiled or inadequately refrigerated fish/shellfish. This reaction is due to the presence of naturally-occuring histidine in fish or shellfish. As the seafood spoils, bacteria grow rapidly and convert histidine to histamine. Ingestion of histamine can cause a pharmacologic reaction in susceptible individuals that mimics the symptoms of allergies. Symptoms of scombroid poisoning can closely resemble a typical IgE-mediated allergic reaction, including nausea, vomiting, facial flushing, respiratory symptoms, itching and hives. Treatment includes administration of fluids, antihistamines, oral steroids, and at times epinephrine.
Ciguatera Poisoning
Ciguatera fish poisoning is a similar appearing acute reaction to scombroid poisoning, but this poisoning is caused by Ciguatera toxins. These toxins are often found in larger predator fish, such as barracuda, red snappers, eels, sea bass, and Spanish mackerels. This is a commonly unreported or misidentified condition, but can have significant consequences. These reactions are often confused with allergic reactions to the predator fish, with symptoms including dizziness, abdominal cramps, vomiting and hypotension.
Testing for shellfish allergy
Skin testing is often recommended as a first method of evaluation of shellfish allergy. Interpretation can be difficult due to potential cross-reactivity between types of seafood or between shellfish and dust mites. Skin tests with commercial seafood extracts usually show reliable results, but if there is uncertainty, the actual food can be used. Commercial seafood extracts may also run the risk of false negatives, because the extracts often only have the major allergen tropomyosin and not the secondary allergens like myosin light chain protein and hemocyanin. Dust mites and other cross-reactive species do possess the secondary allergens that can sensitize an individual, making them more susceptible to a subsequent allergic shellfish reaction. So, it is important to test for reactions to dust mites and cockroaches, otherwise the skin testing may be incomplete and lead to falsely negative results.
Food challenges may also be done, most often when skin tests and/or history is inconclusive.
Unorthodox testing is available for food allergy, but is not recommended. Examples of this type of testing includes use of electrodes (Vega testing), cytotoxic testing (Bryan’s test), iris examination (iridology), IgG food antibody testing, hair analysis and more. In addition to being ineffective, these tests can lead to negative consequences for the patient such as unnecessary dietary restrictions and false confidence about protection from allergies.
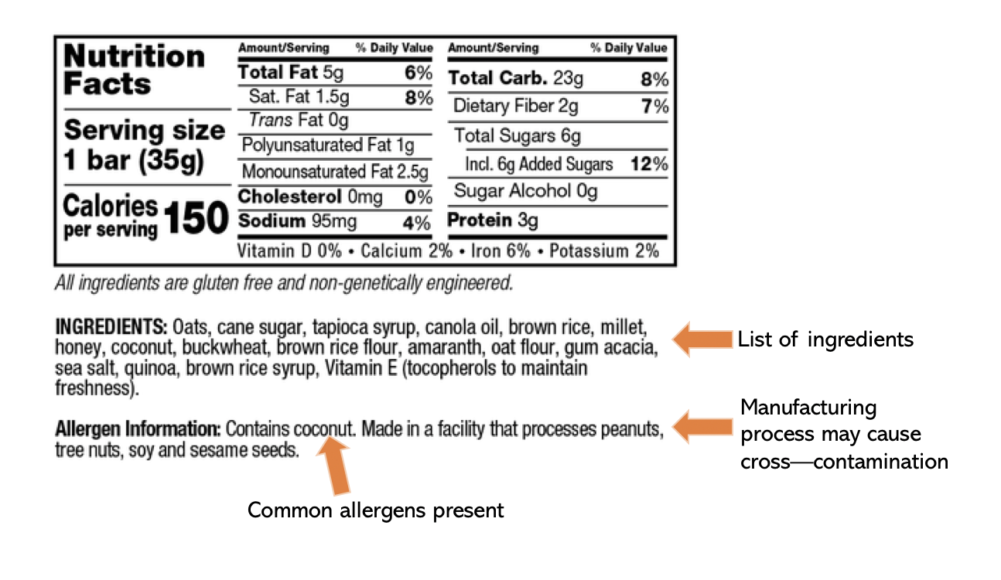
Treatment for shellfish allergy
Allergy to shellfish is usually not outgrown and persistent throughout life. The first line of treatment is thus strict avoidance of shellfish. A major part of this includes avoidance of foods that can potentially be cross-contaminated with shellfish. For example, grocery stores or restaurants where foods can contain unexpected derivatives of shellfish, like in stocks or oils used to prepare the foods. It is important to always ask the person preparing the food if there is risk of hidden exposure. Those with food allergies should also always carry self-injectable epinephrine to treat serious reactions from accidental exposures.
More Info
December 28, 2020. How Humidifiers Can Help Your Home
It is estimated that in industrialized countries, residents spend over 90% of their lives indoors. A statistic like this also indicates the importance of indoor air quality on one’s health.
What are common causes of poor indoor air quality?
Air quality can cause new respiratory symptoms or exacerbate present ones. These problems can be more common than one might expect; some studies report that up to 60% of workers have experienced at least one environment or building-quality related symptom at work (although there is no standardized diagnosis). Common sources of pollutants of air quality include mold, secondhand smoke, cleaning products, dust mites, cockroaches, plant pollen, rodents, hair or fur from domestic animals and more. Proper ventilation and filtration can help reduce the effects of these pollutants in indoor air.
What are common symptoms that result?
Another important component of indoor air quality is humidity, which can impact skin and respiratory tract health. Dry air can cause dry nose, dry lips, throat or skin irritation, nasal bleeding or crusting, sore throat, and potentially cough. Normally functioning mucous membranes seem to require around 35-45% relative humidity. Poorly humidified homes can also affect wood furniture by increasing separation of wood, wood floors due to shrinking and expanding of wooden planks, peeling of wallpaper and covering, plant damage and increased dust.
What can I do to fix this problem?
A common remedy to this problem is purchasing a humidifier or vaporizer for the home that helps add moisture back into the air and avoid some of the less-than-ideal symptoms of dry air. The two types of humidifiers are warm mist or cool mist humidifiers. Warm mist humidifiers heat water to a boil before releasing it as mist into the air. These are considered healthier for circulating air, as the boiling water can help kill bacteria and mold before they are released into the air. But, these are also usually more expensive and work better in smaller rooms. Cool mist humidifiers do not heat water before releasing it. For some, these are preferred because they are more suited to larger rooms, use less energy, and are potentially safer than warm mist humidifiers. However, these can emit bacteria, molds, and white dust into the air.
Ultrasonic humidifiers
These humidifiers can be of either warm mist or cool mist type. These are quiet filters that use high frequency ultrasonic vibrations to mist the water. These are considered low-maintenance, low-energy (no heat is used), portable and good for small rooms. However, these also run the risk of spreading bacteria if tap water or any sort of mineralized water is used.
Evaporative humidifiers
These humidifiers are the most common type of humidifier used. In these, water is absorbed by a wick filter and is then dispersed into the air by a fan. These do not contaminate the air as much as some other types of humidifiers may, but these may still produce a significant amount of noise.
Central humidifiers can also be used, as they are connected to the home’s air heating system. This humidifier can add moisture to the ventilating air as it passes through. However, these may not add sufficient humidity to a room like a bedroom.
Using Your Humidifier Effectively
Whether you have a humidifier already or are planning on purchasing one, here are some key tips to ensure efficacy and efficiency of your humidifier:
- Clean your humidifier thoroughly before, during, and after heating season.
- Try using vinegar rinses or a teaspoon of bleach in a gallon of water. Leave for 20 minutes and use the manufacturer’s cleaning instructions.
- Avoid leaving stagnant pools of water, as these are good places for germ and mold breeding.
- Use distilled water instead of tap water when you can.
- Do not add anything else to your humidifier (ex. Vick’s VapoRub, oils, …)
- Consider the size of the unit and ensure that you have enough water to satisfy it.
- Invest in a humidifier that is properly made and corrosion-proof.
- Remember to turn off the water supply, drain and clean reservoir pan for humidifiers in central heating systems when the heating season is over. Keep track of the waterline feed for the central heating system by checking on it at least once or twice a season.
- Keep a hygrometer (a device to measure humidity) in your bedroom to track the room’s humidification. Ideal humidity is around 35-45%.
- Remember that relative humidity above 55% encourages growth of mold/bacteria.
- Keep steam or warm mist humidifiers out of reach for children to avoid injury from hot water.
- Do not let the area around the humidifier get wet.
More Info

December 21, 2020. Christmas Tree Allergies – Bah Hum “Bugs”, Not Really
By Dr. Marc F. Goldstein, Board-Certified Allergist at The Asthma Center (Philadelphia PA, Mt. Laurel NJ)
Are Christmas tree allergies getting in the way of the “most wonderful time of the year?” Read on for some easy fixes for this common problem:
Many allergy sufferers see increased allergies during the holiday season. Common problems of “Christmas Tree Syndrome” include:
- release of allergic evergreen pollen and other pollens embedded in tree cones
- mold at the base of the tree
- dust from old decorations
- and many more.
In fact, a 2011 study found that more than 50 types of mold were found on researchers’ own Christmas trees, 70% of which could be potentially harmful to those with allergies. Symptoms of these allergies that often arise include nose congestion, itching, water discharge and/or repeated sneezing.
A similar reaction can also occur in response to pine pollen or other pollen trapped in pine cones. Some may experience contact skin reactions (rashes, itchy skin) after touching tree needles or sap. Good ways to avoid/minimize this reaction are to use gloves when handling the tree, shake the tree vigorously, and hose it down before use.
Poinsettias are also popular holiday flowers that have a component similar to latex and thus skin contact with these can aggravate people with latex allergies as well.
Top 8 Tips to Avoid Christmas Tree Allergies & Asthma
- Clean Your Christmas Tree. Before you bring your Christmas tree inside, be sure to shake it out, rinse it off with a hose, and let it dry! With fresh cut trees, pay special attention to the bottom of the tree because this is where the most pollen, dirt and mold are found. With artificial trees, dust which may have collected throughout the year can be a potential allergy & asthma trigger as well, so be sure to clean these trees before decorating.
- Minimize the time that your tree is inside the house. Try waiting until a few days before Christmas to bring the tree inside, and removing it one to two days after Christmas.
- Dust and Clean ornaments, wreathes, and garlands before decorating. As with Christmas trees, dust on ornaments can trigger symptoms as well. When storing them again after the holiday season, use an airtight container and store in a dry spot, if possible.
- Consider using an artificial tree. Be sure to dust and clean this, for example by using a damp cloth, as well before using. Avoid spraying pine scent or fragrance on the tree.
- Avoid scented candles, pot pourri and aerosol sprays. These can irritate the noses and throats of people with allergies.
- Avoid fireplaces, ash & smoke–this can present particular problems for those with asthma.
- Avoid touching wreathes, garlands and trees if you have sensitive skin or severe allergies. This can result in a red/itchy rash (contact dermatitis).
- If you are going to another person’s house for a socially distanced gathering, there is still a chance of developing allergic reactions to the host’s trees and holiday decorations. Try discussing a plan with your allergist before you go; this might include taking something like an antihistamine before you go.
Christmas Tree Bugs
A recent report estimates that a single Christmas tree could be infested with thousands of bugs including aphids, spiders and mites, bark beetles, praying mantises, and more! While unwanted and perhaps unpleasant, these microscopic insects are often not health threats. To avoid these, we recommend letting fresh trees sit inside your garage for at least one day before bringing it inside. Additionally, some individuals find it helpful to spray organic neem oil on a Christmas tree. This oil can kill bugs in all stages (from eggs to adults). A diluted form of bleach (try one part bleach to 20 parts water) on trees can help kill mold and insects. The smell of bleach, however, can also be irritating to the airways.
How Allergists Can Help
Board-certified adult and pediatric allergists can help patients minimize Christmas allergies, asthma, and sinus problems. Using minimally invasive in-house diagnostics, like allergy skin testing, breathing tests, and knowledge of local allergy triggers like dust, pine tree pollen, ragweed and mold, our allergists at The Asthma Center can develop personalized plans that treat not only the symptoms but also find the cause of allergies. Several treatment options, including allergy immunotherapy, are effective and offer non-drowsy solutions. The board-certified allergy and asthma specialists at The Asthma Center treat patients in 4 convenient locations throughout the Delaware Valley.
More Info
December 11, 2020. Allergic Reactions and The Coronavirus COVID-19 Vaccine: Is It Safe If I Have Severe Allergies?
By Dr. Marc F. Goldstein, Board-Certified Allergist at The Asthma Center (Philadelphia PA, Mt. Laurel NJ)
As the coronavirus (COVID-19) pandemic continues, there has been significant progress on the development of a COVID-19 vaccine. Will the coronavirus vaccines be safe to take for people with severe allergies (like peanut allergies, egg allergies or other food allergens)?
Do People Who Get The Coronavirus (COVID-19) Vaccine Get Allergic Reactions?
In the United Kingdom, there were two reported cases of severe allergic reactions occurring during the first day of public vaccination in the United Kingdom which have set off a flurry of questions about the safety of coronavirus (COVID-19) vaccines in individuals with a history of allergic reactions. The two individuals who suffered allergic reactions had a history of significant allergies (the nature of their allergic reactions and triggers have not been reported). The two patients recovered after treatment which may have included use of epinephrine.
How Common Is An Allergic Reaction to The Coronavirus (COVID-19) Vaccine?
Allergic reactions to vaccines, including a severe life-threatening anaphylactic reaction to a vaccine, are anticipated with any vaccine just as with drugs, but they are rare events. From large epidemiologic studies, anaphylaxis after vaccination occurs at a rate of 1.31 cases for every one million vaccine doses given. During the late stage clinical trials of the Pfizer/BioNTech COVID-19 vaccine clinical trials, there were 42,000 patients who received the vaccine administered in two doses and the allergic reaction rate was 0.63% in those who received the vaccine compared to 0.51% in those who received placebo. This difference was not statistically significant. This means that just about as many people had reactions to the placebo as had reactions to the vaccine. The severity and the nature of the reactions have not yet been reported. Patients who had a history of severe allergic reactions notably were excluded from participating in the clinical trial. People with common environmental allergies were not excluded from the study. Patients with common food allergies were also not excluded from the study because there is no trace of eggs, peanuts, tree nuts or other food protein in the vaccine.
Is It Safe To Get The COVID-19 Vaccine If I Have Severe Allergies?
As a consequence to the two reported cases of allergic reactions to the COVID-19 mRNA vaccine in United Kingdom, the United Kingdom Medical and Healthcare Products Regulatory Agency which sanctioned the use of the vaccine under emergency authorization in the UK, came out with a statement which said that people with a history of allergic reactions (significant reactions to vaccines, medicines, and foods) or a history of near fatal allergic reactions (anaphylaxis) should not receive the vaccine. This prohibitory precaution may, however, be an overreaction to the true risk of allergic reactions to the COVID-19 vaccines in the general public or to people who have had prior allergic reactions to medication and/or vaccines or have a history of anaphylaxis.
What Causes The Allergic Reaction in The COVID-19 Vaccine?
In general, allergic reactions to vaccines most commonly have been attributed to additional inactive components within vaccines like gelatin, egg protein, thimerosal, formaldehyde, possibly latex found in the rubber stoppers of vaccine bottles, and other possible excipients (inactive substances that serve as a vehicle or medium for an active substance like coloring agents, preservative, and fillers). Fatalities to vaccines have rarely been reported. The unique Pfizer vaccine has nucleoside modified messenger RNA genetic material which in itself is unlikely to produce an allergic reaction due to its size and structure. The messenger RNA is packaged in a lipid nanoparticle which holds the messenger RNA along with excipients including polyethylene glycol, sucrose, and a variety of salts. The lipid nanoparticle and salts are unlikely also to cause allergic responses in as much as these materials or similar materials are found naturally in the body and do not cause allergic reactions. Polyethylene glycol on the other hand has on occasion been reported as a cause of allergic reactions in some individuals.
How And Where Should I Get The COVID-19 Vaccine Safely If I Have Severe Allergies To Eggs or Peanuts or Other Allergens?
The COVID-19 vaccine, like all other vaccines, should be administered in a facility that can treat an allergic reaction if it occurs and as a precaution, the patient should routinely wait 20 to 30 minutes after vaccine administration in such a facility. Despite the United Kingdom statement, there may not be enough data at this point to justify the exclusion of patients who have a history of allergic reactions to foods, drugs, environmental allergens, or other vaccines, from COVID-19 vaccination. In fact, the FDA, after approving the Pfizer vaccine for emergency use, stated that the Pfizer coronavirus vaccine appears to be safe for people with food or environmental allergies. The only allergic warning is limited to a prior allergic reaction to the vaccine itself and/or an allergic reaction to a vaccine component. This warning is consistent with allergic warnings for other vaccines.
Patients who have a history of allergic reactions should inform their providers before getting vaccinated and they should receive the vaccine at a place where they can be observed for any adverse reaction for at least 20 minutes after the vaccine is administered. The facility should also have the capability of treating a severe allergic reaction. Though continued surveillance of adverse reactions, including allergic reactions, will be essential during the rollout of the new COVID-19 vaccines, based on the current available data, individuals with a history of allergic reactions should still consider taking the COVID-19 vaccine. However, anyone who has specific allergy concerns regarding the vaccine should speak with a knowledgeable board certified allergist.
Copyright (c) 2020
No reprints without written approval from Allergic Disease Associates, PC (The Asthma Center)
More Info
December 1, 2020. Penicillin Allergy: Less Common Than It Seems
Penicillin allergy is one of the more commonly reported medication allergies, affecting up to 10% of all patients and 15% of hospitalized patients. But, many such individuals may not actually be allergic, as some individuals lose sensitivity as they age. Fortunately, there is a way to learn whether you have lost your penicillin sensitivity and can be de-labelled as penicillin-allergic.
“Penicillin” actually refers to a group of antibiotics that are used to treat bacterial infections (including sinus, ear, respiratory, skin, and more). Penicillin antibiotics are a subgroup of a larger class of beta-lactam antibiotics. Beta-lactam antibiotics in general are used to eliminate different types of infectious bacteria. There are several types of allergy to penicillin and these vary by severity and onset of the reaction; the most common are immediate versus delayed reactions.
Immediate Hypersensitivity
Immediate hypersensitivity to penicillin drugs is due to the interaction of penicillin-specific IgE antibodies (allergy antibodies) with mast cells (immune-sensitized cells in the nose, eyes, chest, lungs, and more). Naturally, penicillin in its whole form is not very allergenic, but when in the body, it can spontaneously break down and create more allergenic intermediates. These intermediates, called major and minor determinants, can induce the formation of specific IgE antibodies, which then bind to mast cells and basophils in a process known as sensitization. Sensitization itself is usually asymptomatic. But, with re-exposure to penicillin after this sensitization, the IgE antibodies on mast cells and basophils will trigger an immune response when bound to penicillin allergens. The allergic response is based on the release of histamine, leukotrienes, and other common inflammatory chemicals, from the mast cells.
Symptoms of an immediate immune response typically begin within one hour of exposure to the drug. These symptoms can be severe, including:
- Itching (pruritus) or hives (urticaria)
- Swelling of the larynx in the respiratory pathway (laryngeal edema)
- Tightening of muscles in lungs (bronchospasm)
- Significant drop in blood pressure (hypovolemic shock or hypotension)
- Wheezing or coughing
- Nasal congestion
- Deep swelling in various body parts (angioedema)
- Nausea/vomiting/diarrhea
- Feeling dizzy or light-headed
- Irregular heartbeat
A more severe or potentially life-threatening reaction is anaphylaxis, which can cause any of the above symptoms, often with low blood pressure.
Risk factors contributing to potential immediate allergy to penicillin include: age (20-49 y/o), frequent intermittent exposure to penicillin, parenteral administration (injection of penicillin directly into the bloodstream or muscle), having multiple antibiotic allergy syndrome (allergic reactions to multiple classes of antibiotics), being closely related to another individual with antibiotic allergies, and having other allergies in general.
Delayed Hypersensitivity
Delayed hypersensitivity to penicillin is very different from immediate hypersensitivity. Symptoms of delayed hypersensitivity occur after multiple doses, for example after being on penicillin treatment for several days. In addition, the mechanism of reaction is different from that of immediate hypersensitivity; these reactions are not IgE-mediated but instead can occur through several different mechanisms. Usually these reactions are not life-threatening.
Delayed hypersensitivity symptoms can also include:
- Itching (pruritus) or hives (urticaria)
- Swelling around the body (angioedema)
- Rashes (erythematous macules/papules)
Why Should You Get Tested?
Being able to use penicillin for a bacterial infection is very beneficial. Penicillin is itself inexpensive and often effective in the case of non-penicillin resistant bacteria; penicillin alternatives have been associated with increased healthcare cost and longer hospital stays.
Testing Procedures
Testing and evaluating a true penicillin allergy begins with taking a clinical history and, if suspicious about an allergic reaction, performing skin tests. If the skin test is positive for penicillin, then avoidance or desensitization of penicillin is recommended. If the skin test is negative even with a suspected positive history, an oral challenge is used to ensure that penicillin can in fact be tolerated by the patient.
Penicillin is actually one of the few drugs that has accurate and predictive skin tests available. A skin test works by detecting the presence (or lack of) IgE antibodies in response to the specific allergen that is introduced to the skin. Allergen-specific IgEs will be present on skin mast cells in an individual who is currently penicillin allergic. A skin test positive to penicillin will reflect a local allergic immune response by resulting in small red bumps or hives. From here, treatment will include use of a non-penicillin antibiotic or a penicillin desensitization regimen can be discussed if there are no alternatives to penicillin.
Skin tests are usually performed either as prick tests or intradermal tests. A prick test exposes the patient’s skin to a small amount of allergen using a small prick to the skin. If the test is positive, hives will form at the site of exposure and will vary in size depending on the patient’s sensitivity to the allergen. For a complete evaluation, minor and major determinants of penicillin allergy should be included in the testing. It has been shown that using only the major determinant (PPL) in the skin test can be less accurate than using a combination of minor and major determinants. Intradermal tests are much more sensitive and are conducted using a very small injection in the patient’s upper arm; these are used if prick tests are negative. These tests usually take about one hour. Antihistamines should be avoided for 3 days prior, because these can interfere with the skin test results. A common and beneficial place to get tested is at an allergist’s practice. Interpretation and evaluation of skin testing should be done by an allergy specialist.
Although both skin testing and blood testing have diagnostic challenges, skin testing is still more accurate than blood testing and thus the preferred option. In addition, commercial blood testing does not include all relevant allergic penicillin determinants and a negative blood test can be misleading.
Another important component of evaluation of penicillin allergies is the time between testing and occurrence of last allergic reaction. Penicillin-specific IgEs decrease over time, meaning that individuals with more recent reactions will likely be more allergic than those with more distant reactions. Additionally, a good time to conduct this testing is when the patient is currently well and not in need of urgent penicillin treatment. Skin testing is rapid, cost-effective, and safe.
Desensitizations
Desensitization therapy is used to temporarily induce tolerance to the allergen, in this case penicillin. Desensitization can be important for patients who require the use of a specific medicine to which they had a prior reaction. This process induces tolerance by taking a small amount of allergic drug gradually, using a series of dilutions, starting at very low concentrations and building tolerance by progressively increasing the dosage at specified time intervals. The procedure is completed under clinical supervision in an allergist’s office, with blood pressure, pulse oximetry, and breathing monitored. The oral route is preferred as it is generally considered safer than injection directly into the bloodstream.
Treatment using alternative drugs in individuals with penicillin allergy
Cephalosporins are antibiotics within the beta-lactam class (like penicillin) that share many similarities with penicillin. Although rates of cross-reactive reactions of cephalosporins with penicillin are low, especially with the newer generations of cephalosporins, cephalosporin reactions still occur and can be severe. Therefore, cephalosporin antibiotics should only be used in penicillin allergic individuals after careful risk assessment. Skin testing for cephalosporins has been explored, but is usually not as well-validated as skin testing for penicillin.
On the other hand, monobactams are beta-lactam antibiotics as well and are also structurally similar to penicillin, but do not show significant cross reactivity with penicillin, allowing monobactams (i.e. aztreonam, ceftazidime) to be given to patients who have penicillin allergy.
More Info

November 17, 2020. Understanding Food Allergies and Intolerances (They’re not the same!)
Food allergies and food intolerances are new to almost no one. Most know about the common struggles and discomfort that each of these bring, but not many know about the differences between allergies and intolerances and the difficulties of treating each. Here’s our basic guide to understanding food allergies, food intolerances, and more.
What are food allergies?
Food allergies, although they seem incredibly common, only affect about 1-2% of the adult population and up to 6% of children [1]. Common food allergies include peanuts, tree nuts, milk, eggs, and shellfish. Symptoms can vary in type, location in the body, severity, duration and more.
Food allergies can be seen as the body’s defense mechanism acting in response to foods that, under normal circumstances, do not produce reactions. In those who do have allergic reactions, the immune system recognizes certain protein signals on the food, which the body then sees as the foreign invader [9]. The molecule that recognizes these protein signals is called an “antibody” or “immunoglobulin” (Ig), in this case IgE. This causes allergic reactions in some food sensitive people as the body tries to “eliminate” the food that it sees as foreign.
Common symptoms are usually gastrointestinal (GI) or cutaneous (related to the skin). The gastrointestinal tract lining is your digestive system’s barrier between the outside environment and the body’s internal processing space for absorbing nutrients from food. Allergic inflammation in the GI barrier can cause discomfort through symptoms like diarrhea, vomiting and abdominal pain [2]. Cutaneous symptoms can include acute urticaria (hives), angioedema (fluid swelling beneath the skin) and contact dermatitis after handling food (presents as red itchy rash on skin but is not contagious). Experiencing respiratory symptoms as a result of food allergy is less common, but symptoms can include food-induced nasal congestion, runny nose and wheezing [3]. Food allergy symptoms are due to the release of naturally occurring histamine. Histamine is produced by mast cells that live in different tissues of our bodies. Mast cells are usually found at interfaces where the body meets the outside environment, for example in the lungs, nose, eyes, or skin. When a substance from the environment reaches the barrier and is recognized as foreign, the IgE on the surface of the mast cell binds the allergen [10], allowing for activation of mast cells that release histamine and other allergic inflammatory chemicals, such as leukotrienes that amplify the allergic response.
Oral allergy syndrome is easy to confuse with a food allergy, but there are important differences. Oral allergy syndrome often occurs in individuals who already experience seasonal allergy symptoms (itchy eyes, itchy nose, nasal congestion). Their bodies undergo allergic reaction in the presence of pollen in the air. In oral allergy syndrome, certain food proteins cross-react with pollen proteins, telling the body to react as if you were eating the pollen itself. Symptoms are usually limited to itching or swelling on or around the mouth and resolve themselves with time. Treatments often include avoidance of certain foods. Common cross-reacting pollen-food pairs include:
- Ragweed pollen cross-reacts with bananas, cucumbers, melons, sunflower seeds, zucchini
- Grass pollen cross-reacts with celery, melons, oranges, peaches, tomato
- Birch pollen cross-reacts with apple, almond, carrot, celery, cherry, hazelnut, kiwi, peach, pear, plum
What are food intolerances?
Food intolerances create a reaction using a different mechanism than allergies. Food intolerances do not operate through the IgE antibody, but instead by pharmacologic or toxic substances in the food or other non-IgE immune mechanisms [9]. For example, touching or ingestion of external sources of histamine (like spoiled or poorly refrigerated fish) can cause allergy-like symptoms. This is a form of pharmacological reaction rather than actual allergy to fish [5].
Another more common example of a food intolerance is lactose intolerance, making it difficult to consume cow’s milk daily products (like cheese or ice cream). Again, this is not due to an IgE-mediated reaction but rather due to a digestive enzyme, lactase, that some individuals do not have. Treatments for lactose intolerance include avoidance of dairy, using no-lactose alternatives, or lactase supplements.
Some other common non-allergic food intolerances include sensitivities to carbohydrates (specifically to fermentable oligo- di- monosaccharide polyols, also known as FODMAPs) or gluten, a common protein found in rye, barley, oats, wheat and more. Sensitivity to these can induce gastrointestinal symptoms of abdominal pain, bloating, flatulence, and more [1].
Celiac disease (CD) is a specific immune disorder that can also cause discomfort and pain after eating gluten. When a patient with CD eats gluten, the body produces an immune response on itself in order to try and eliminate the gluten that it sees as foreign. CD is often misdiagnosed as irritable bowel syndrome or wheat intolerance/sensitivity. Irritable bowel syndrome (IBS) is also an example of a common food intolerance that can cause abdominal cramping, bloating, and bowel irritation. IBS can also be triggered by highly fatty meals, coffee, alcohol, excessive fructose or sorbitol (two types of sugar). These symptoms are again related more to digestive system reactions rather than immune system reactions. CD is also hereditary, meaning it is passed through families. Treatment includes changing to a gluten-free diet. Although some symptoms may be similar, CD is different from wheat intolerance (non-Celiac gluten disease) which is also different from wheat allergy. Non-Celiac gluten disease (NCGD), or non-Celiac wheat sensitivity, is neither an autoimmune disorder (like CD) nor an IgE-mediated immune reaction (like wheat allergy). Treatment usually also includes identifying the threshold amount of gluten to initiate symptoms and avoidance of gluten. Wheat allergies are IgE-mediated allergic reactions to wheat allergens.
How do you test for food allergies and intolerances?
The current gold standard for food allergy testing is conducting a double-bind placebo-controlled trial [1], which is a way to clinically rule out or rule in specific food allergies. However, this is an expensive and time-consuming process and is not always feasible. A food challenge can also be done by eating small amounts of specific foods under clinical supervision and watching for reactions. More practically, skin prick tests can be used to test for allergies. Skin testing determines whether the allergic symptoms are due to presence of allergen-specific IgE antibodies [7].
How do you treat food allergies and intolerances?
The first method and most common starting point is often avoidance of certain foods from the individual’s diet and patient education about how to do so. Patients can work with dieticians to ensure they are not over-restricting themselves in their diet. Medication can be used to mitigate symptoms. In the case of accidental exposure leading to severe reactions, adrenaline/epinephrine (such as an EpiPen) or antihistamines should always be available.
Understanding how to read food labels and recognizing uncommon names for ingredients is critical to successful avoidance of specific allergens. For example, gluten is found in many common foods, including wheat, oats, barley, brown rice and rye. Gluten may also be found in beer, soy sauce, teriyaki sauce, and broth. It is always good to check with the manufacturer or chef if you are unsure about whether something has gluten in it or not, either as an ingredient or through potential cross-contamination. Gluten alternatives usually include almond flour, buckwheat flour and coconut flour. If the food’s ingredients say “Gluten-Free” then the product is usually safe (FDA labels gluten-free as foods with less than 20ppm gluten present). However, it is important to remember that “wheat-free” is not the same as gluten-free. Check the rest of the ingredients to make sure there are no hidden allergens.
Lactose, like gluten, also comes in many less-recognized forms. Lactose, whey and casein are all major components of milk and dairy, meaning that isolation of whey or casein proteins can still contain lactose. Usually lactose is only present in small amounts, but for those with severe lactose intolerance, whey and casein should still be avoided. Whey is popular as a dry protein powder, so many individuals with lactose intolerance turn to non-dairy protein powders like soy or pea protein. Lactose can also be found in medications, such as vitamin D pills or birth control. Although it is usually found in small amounts, it would be best to check with your doctor before using lactose-containing medication if you are intolerant.
In some cases, desensitization to the food allergen can occur. For example, peanut allergies can be weakened using oral immunotherapy, which controls exposure to peanuts overtime with the goal of increasing the threshold of peanut ingestion before reaction. This is done in an allergist’s office equipped to treat anaphylaxis. The patient should also continue to carry epinephrine because this is not a cure for food allergy.
More Info
November 3, 2020. the Flu (influenza): Symptoms, Vaccines, and Treatments
By Dr. Marc Goldstein
The “flu” is short for influenza virus that can cause infection in the upper respiratory tract and lungs. The illness that people call the “stomach flu” is almost never caused by influenza. The symptoms of influenza include fever, headache, chills, and cough often followed by generalized aches. Fever is usually high grade (103° F) and may last for 3 to 4 days. Sometimes people also experience runny nose, sneezing, sore throat, or tightness in the chest. Most people recover within a week but may continue to feel exhausted or just not themselves for several weeks.
Flu is generally passed from one person to another by sneezing or coughing. The virus can live for a short time on objects. For this reason, you can come down with influenza by touching something that has been handled by someone who is already infected and then touching your mouth, nose, or eyes. Flu influenza spreads easily and quickly, especially among schoolchildren, their families, and among people who live in crowded conditions. After the virus enters your body, you may have no symptoms for 2 to 4 days. But after symptoms appear, you may spread the virus at least for 3 to 4 days.
There are estimated 5 to 20% of Americans affected each year with seasonal influenza. The incidence of influenza related deaths in the US ranges from 3,000 to 40,000 per year with another 200,000 people hospitalized. The flu is less contagious and has less fatalities than that associated with the current COVID-19 pandemic. However, influenza, like COVID-19, can cause serious complications. In high risk populations, influenza can lead to bacterial pneumonia that can be life threatening. In children, Reye’s syndrome is a serious liver and brain disorder that has been linked to the use of aspirin in children affected with influenza virus.
Who should be vaccinated? Annual vaccination against influenza A and B virus is recommended for everyone 6 months or older without a contraindication. Vaccination can reduce the prevalence of influenza illness and symptoms that may be confused with those of COVID-19. A variety of vaccines are available. The optimum time for a vaccine is from October through the end of November, and although there is no guarantee you will not get influenza, the vaccine can greatly reduce your chance of getting the disease or having a severe case.
Because eggs, thimerosal, formaldehydes and other excipients are used in some injectable flu vaccinations, be sure to tell your doctor if you have allergies to these items. Allergy to egg, however, is not associated with allergic reactions. In 28 studies that have included over 4000 patients with egg allergy (over 650 with a history of severe allergic reactions), there were no reports of anaphylaxis after administration of egg-based inactivated influenza vaccines, although some mild reactions did occur. Currently, any age-appropriate influenza vaccine can be administered to persons who report a history of hives related to egg exposure. People with more severe egg allergies may also receive an age-appropriate influenza vaccine in a healthcare setting that can treat severe allergic reactions. Desensitization protocols are performed in our office for this purpose. The recombinant vaccine from cell culture-based inactivated vaccines are not prepared in chick embryos and therefore do not have egg protein.
The composition of the influenza vaccines may vary. Trivalent vaccines contain only 1 influenza B virus and 2 strains of influenza A virus. Quadrivalent vaccinations contain 2 influenza A and 2 influenza B strains. For patients 65 years and older, a high-dose vaccine is recommended. This year high-dose vaccines include inactivated quadrivalent vaccine which is 4 times as potent antigenically as the standard quadrivalent vaccine. Observational study has shown that a high-dose vaccine is associated with reduced risk of respiratory disease and hospitalization and death compared to standard-dose vaccines.
Influenza vaccine is also recommended in pregnant women without regard to the trimester of pregnancy. Pregnant women should not receive the live attenuated vaccine, which is available only in an intranasal form called FluMist. This is a quadrivalent vaccine that is recommended for ages 2 through 49 and is also contraindicated in patients who have underlying asthma.
Antiviral drugs for influenza are available. Antiviral drugs should be started as soon as possible. It is most effective when it is started within 48 hours after illness onset. It can be considered for healthy asymptomatic patients with suspected or confirmed influenza who are not at increased risk for complication and can be started within 48 hours after illness onset. Oral oseltamivir, IV peramivir, and inhaled zanamivir, or oral baloxavir can be used for treatment of non-pregnant patients with acute uncomplicated influenza.
Post-exposure prophylaxis (PEP) should be considered for persons with increased risk of influenza complications who have not received an influenza vaccine this season; those who received the vaccination within the previous 2 weeks who might not have immunologically responded to the vaccine, for example those who are immunocompromised or when the match between the vaccine and circulating strain is poor. It is not recommended for healthy persons exposed to influenza or when greater than 48 hours have elapsed since exposure.
Antiviral chemoprophylaxis is recommended in an institutional setting (like nursing homes) to help control influenza outbreaks. Oseltamivir and zanamivir are FDA approved for post exposure prophylaxis. Chemoprophylaxis can be continued for 7 days after the last known exposure in an outpatient setting.
More Info











