Coronavirus vs Asthma: How to Tell The Difference?
by Marc Goldstein, MD, Board-Certified Allergist at The Asthma Center
Do I Have Greater Risk for Getting Coronavirus If I Have Asthma?
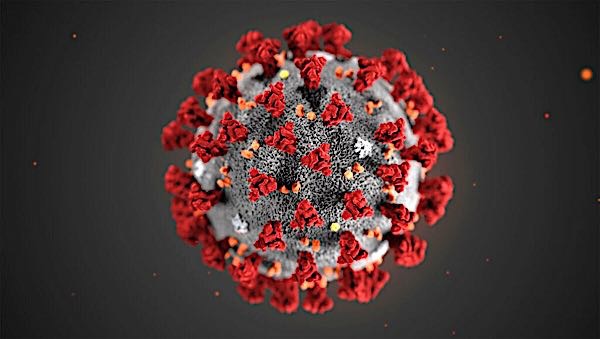
In a time when asthma symptoms may be flaring due to weather changes and seasonal spring pollens, people with asthma may worry whether their asthma may put them at risk for getting coronavirus (COVID-19). It can be confusing because both asthma and coronavirus share symptoms of cough and shortness of breath. The good news that the chance of getting coronavirus for anyone with asthma is really no different than for someone without asthma. Getting coronavirus comes down to an individual’s exposure to suspected or confirmed cases of coronavirus or to symptomatic carrier of SARS-CoV-2 virus (the virus that causes the COVID-19 infection). Therefore, to reduce your risk of getting coronavirus whether you have asthma or not, practice the social distancing, hand washing, mask and glove protection, and surface disinfection that has been promoted by the CDC and public health and infectious disease experts (see more here).
What If I Have Asthma and Coronavirus?
Though asthma does not in itself put you at greater risk to contract coronavirus, those individuals with some forms of asthma may be at risk for complications and may get sicker from coronavirus. The Surgeon General of the United States, recently brought this to the attention of the American public. However, according to the CDC, this concern applies only to individuals with persistent moderate to severe asthma though there is no published data that actually supports this assertion at this time. Fortunately, the vast majority of individuals with asthma have intermittent asthma meaning they have infrequent symptoms and use a rescue inhaler less than 2x/week not including preventative use before exercise. Individuals with moderate persistent asthma are usually on a maintenance inhaler which contains moderate to high doses of inhaled steroids with or without long acting bronchodilators. Individuals with severe persistent asthma are on higher doses of inhaled steroids with or without biologic therapy ( Xolair, Nucala, Dupixent, Fasenra, Cinquair) and have significant limitations in lung function.
Since coronavirus can infect your respiratory tract (nose, throat, lungs), the COVID-19 respiratory virus, like other respiratory viruses like influenza, can precipitate an asthma attack and possibly lead to a viral pneumonia and in the worse case acute respiratory failure from ARDS (acute respiratory distress syndrome.).
How To Tell If My Cough is From Coronavirus or Asthma?
Unfortunately, people can have both asthma and coronavirus. Here are a set of tips to help understand the symptoms that you feel.
- Typical coronavirus symptoms include fever (temperature over 100.4 degrees) , joint or muscle aches and pain, as well as dry cough and significant shortness of breath. Asthma usually does not cause fever unless accompanied by a respiratory infection and usually does not cause the muscle and joint symptoms typical of coronavirus.
- Individuals with asthma often wheeze and feel tightness in the chest. These symptoms are less frequent with COVID -19.
- For those who have had asthma for years and have gone through flares, their symptoms are very familiar. If some of your chest symptoms are atypical for you and you have fever as well, it is worth speaking with your Asthma Center physician as to whether you have COVID 1- 19 and be tested as well as getting your asthma under control. COVID-19 can exacerbate your asthma and it is important to remember andindividual with asthma can experience symptoms from both an asthma flare and from COVID-19.
- Seasonal asthma during the spring may be related to tree and grass pollen, and may also be coupled with allergies in the nose, throat, eyes and ears. With those individuals having typical allergy symptoms in the context of cough and even shortness of breath without fever, the latter symptoms are most likely allergy and asthma and not coronavirus. Coronavirus rarely causes sneezing, runny or stuffy nose. Both conditions can cause loss of smell.
What Is The Most Important Thing To Know If You Have Asthma During Coronavirus?
The most important thing an asthmatic individual should do at this time is make sure their asthma is well controlled and that they follow coronavirus precautions to prevent getting infected. Having your asthma controlled well helps keep your lung function at a higher level allowing you a better chance of getting through coronavirus in your lungs.
Coronavirus decreases the functioning of your lungs. For example, a well-controlled asthmatic with 90% of lung function (without coronavirus) will have an easier time of handling a coronavirus infection in the lungs that decrease lung function to 60%. Compare this to a poorly-controlled asthmatic who starts at 70% of lung function and drops to 40% with a coronavirus pneumonia. Starting at a higher lung function by well-controlling and treating your asthma, will help you better fight a coronavirus infection.
Seeing your health care provider at this time (either through telemedicine or in office) is critical for you to improve your chances to beat coronavirus.
What Are Tips For Asthma Sufferers During Coronavirus?
It is important also that your asthma symptoms are well controlled so that those around you do not misconstrue coughing as a symptom of coronavirus when in fact the cough is non infectious from asthma. The following recommendations are important for those with asthma particularly those with persistent moderate to severe asthma. Following these added precautions will decrease your chance of getting coronavirus and having your asthma flare with coronavirus.
- Keep your asthma well controlled with proper medication and using inhalers properly. This may require seeing your Asthma Center provider in-person or through telemedicine.
- Keep your nose and eyes clear of allergies to prevent allergies from triggering your asthma.
- Do not stop your current asthma medicines or change your medication without speaking with your Asthma Center allergist. Do not stop your inhaled steroid medication. Some individuals stop their inhaled steroids because they are concerned they may suppress their immune system. This is not the case and inhaled steroids are important therapies to reduce asthma symptoms and prevent attacks.
- Make sure you have at least a 30 supply of your current and backup asthma medication on hand in case you need to stay home for a long time.
- Avoid your asthma triggers, which may mean you should only go outside when pollen exposure is least like in the late afternoon or evening or after a rain shower.
- If you are living with cats and or dogs which you are allergic too, your asthma may flare due to spending more time spent indoors and exposure to animal dander. Remove your pets from your bedroom, limit physical contact and run a HEPA filter in your bedroom and other rooms of your home where you spend time.
- During this time, it is natural to feel stressed and anxious which may also trigger your asthma. If you find yourself in this situation family, friends and community leaders may be of support as well as methods of behavioral relaxation which you may find online. For some, connecting with a therapist through telemedicine may also be beneficial.
- If possible, have someone without asthma do the disinfecting and cleaning of surfaces since many cleaning produces may induce asthma. Make sure you are not in the room when disinfectants are applied. Make sure the following surfaces remain clean and disinfected: phone remotes, tables, doorknobs, lights switches, counter tops, handles, desks, keyboards, toilets, faucets and sinks.
- There is some concern that nebulizers if used by people infected with coronavirus may aerosolize viral droplets allowing the virus to stay in the air longer and increasing the risk of infecting others. Some hospitals have abandoned the use of nebulizers for this reason. At home, if you use a nebulizer, it may be of benefit to use it isolated from other household members and run a HEPA filter in the room as well to decrease the risk of infecting other people in your household.
- If chest symptoms develop and do not respond to initial backup medications and/or you have a fever with your chest symptoms, call your healthcare provider. The bottom line for people with asthma during the COVID-19 pandemic is to maintain control of your asthma with proper medication under the guidance of your health care provider. Maintaining social distancing, hand washing, wearing a protective mask and gloves outside your home and surface disinfection,in addition to staying out of the emergency room for asthma flares will improve your chances to get through this outbreak.
The bottom line for people with asthma during the COVID-19 pandemic is maintain control of your asthma with proper medication under the guidance of the allergy and asthma specialist at The Asthma
Center. Maintaining social distancing, hand washing, wearing protective mask and gloves outside your home, surface disinfection, in addition to staying out of the emergency for asthma flares will maximize
your chance of safely getting you through this outbreak.
Telemedicine For Patients
The Asthma Center is available to provide the care you need during the coronavirus outbreak. While our offices are still open for in-person visits, our board-certified allergy and asthma doctors will also be available for telemedicine appointments for patients. Please learn more here or by calling The Asthma Center at 215-569-1111 (in Pennsylvania) or 856-316-0300 (in New Jersey).
The information contained in this article is the sole property of The Asthma Center and may not be repurposed for other use without permission from The Asthma Center.
Recent
Popular